Thrombocythemia and polycythemia are blood disorders characterized by an abnormal increase in platelets and red blood cells, respectively, which can lead to complications such as blood clots, stroke, or heart attack. Understanding the causes, symptoms, and treatment options is crucial for effective management and improving your quality of life. Explore the rest of the article to learn how to identify these conditions and manage their risks effectively.
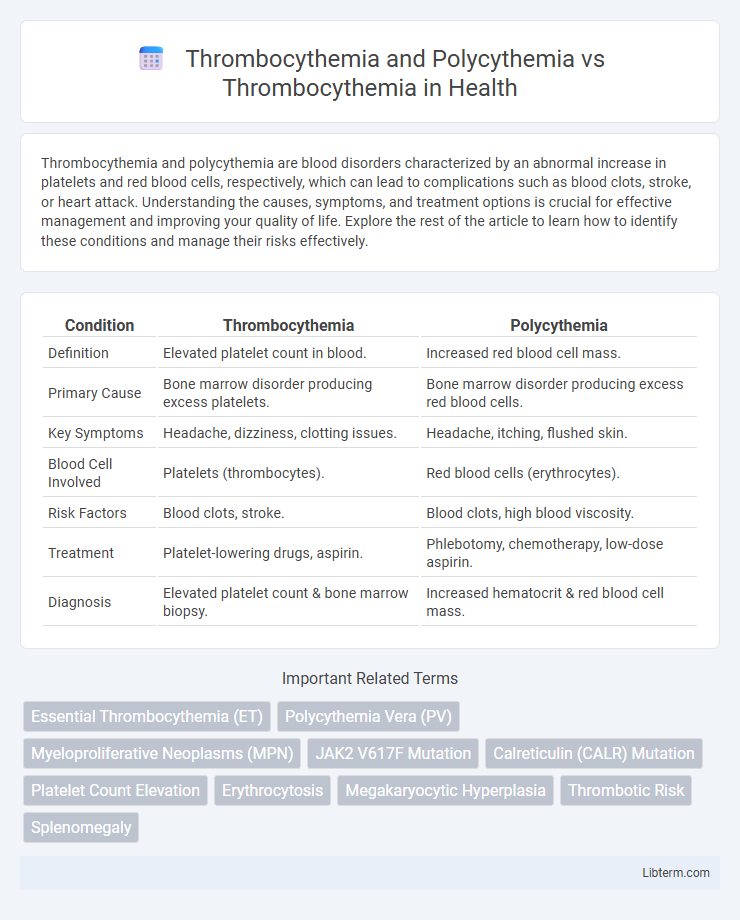
Table of Comparison
| Condition | Thrombocythemia | Polycythemia |
|---|---|---|
| Definition | Elevated platelet count in blood. | Increased red blood cell mass. |
| Primary Cause | Bone marrow disorder producing excess platelets. | Bone marrow disorder producing excess red blood cells. |
| Key Symptoms | Headache, dizziness, clotting issues. | Headache, itching, flushed skin. |
| Blood Cell Involved | Platelets (thrombocytes). | Red blood cells (erythrocytes). |
| Risk Factors | Blood clots, stroke. | Blood clots, high blood viscosity. |
| Treatment | Platelet-lowering drugs, aspirin. | Phlebotomy, chemotherapy, low-dose aspirin. |
| Diagnosis | Elevated platelet count & bone marrow biopsy. | Increased hematocrit & red blood cell mass. |
Understanding Thrombocythemia: An Overview
Thrombocythemia is characterized by an elevated platelet count, leading to increased risk of thrombosis or bleeding complications. Polycythemia involves an excess of red blood cells, causing increased blood viscosity and potential cardiovascular issues, which differs from thrombocythemia's platelet-driven pathology. Understanding thrombocythemia requires recognizing its role in abnormal clot formation and differentiating it from polycythemia to ensure accurate diagnosis and treatment.
What is Polycythemia? Key Facts
Polycythemia is a blood disorder characterized by an increased number of red blood cells, leading to thicker blood and a higher risk of clotting complications. Key facts include its classification into primary polycythemia (polycythemia vera), a myeloproliferative neoplasm driven by mutations in the JAK2 gene, and secondary polycythemia, caused by chronic hypoxia or tumors producing erythropoietin. Unlike thrombocythemia, which involves an overproduction of platelets, polycythemia primarily affects erythrocytes, impacting oxygen delivery and increasing thrombotic risk.
Thrombocythemia vs Polycythemia: Core Differences
Thrombocythemia is characterized by an abnormally high platelet count leading to increased risk of clotting, while polycythemia primarily involves an excess of red blood cells, resulting in increased blood viscosity and potential for vascular complications. The key difference lies in the affected cell line: thrombocythemia targets megakaryocyte proliferation causing elevated platelets, whereas polycythemia causes erythrocytosis with elevated hematocrit and hemoglobin levels. Diagnosis and management focus on cell counts and symptoms specific to platelet dysfunction in thrombocythemia versus oxygen delivery issues and thrombosis risk in polycythemia.
Causes of Thrombocythemia Explained
Thrombocythemia, characterized by an elevated platelet count, can be classified as primary or secondary, with primary thrombocythemia caused by genetic mutations such as JAK2, CALR, and MPL leading to uncontrolled platelet production in the bone marrow. Secondary thrombocythemia arises due to external factors like inflammation, infection, iron deficiency, or malignancies, causing reactive increases in platelet count. In contrast, polycythemia involves an increased red blood cell mass, often linked to mutations affecting erythropoiesis, distinguishing its pathophysiology from thrombocythemia's platelet-focused disorder.
Causes of Polycythemia: Primary vs Secondary
Polycythemia involves an increased red blood cell mass and is classified as primary when caused by genetic mutations in hematopoietic stem cells, such as JAK2 V617F mutation, leading to uncontrolled erythrocyte production. Secondary polycythemia results from elevated erythropoietin levels due to chronic hypoxia, tumors producing erythropoietin, or exogenous factors like high altitude exposure. Thrombocythemia, in contrast, primarily features excessive platelet production typically driven by megakaryocyte proliferation and can coexist with or occur independently of polycythemia.
Symptoms: Comparing Thrombocythemia and Polycythemia
Thrombocythemia primarily presents with symptoms such as frequent headaches, dizziness, and an increased risk of abnormal blood clotting, leading to stroke or heart attack. Polycythemia, in contrast, manifests through symptoms like redness of the skin, especially in the face, fatigue, and elevated blood viscosity causing hypertension and risk of thrombosis. While both conditions involve abnormal blood cell production, thrombocythemia specifically increases platelet count, whereas polycythemia elevates red blood cell volume, influencing their distinct symptom profiles.
Diagnostic Approaches: Thrombocythemia and Polycythemia
Diagnostic approaches for thrombocythemia and polycythemia involve comprehensive blood tests, including complete blood count (CBC) to measure elevated platelet and red blood cell levels respectively. Bone marrow biopsy and genetic testing for mutations such as JAK2, CALR, and MPL are crucial for distinguishing essential thrombocythemia from polycythemia vera and reactive causes. Erythropoietin levels and oxygen saturation tests aid in differentiating primary polycythemia from secondary causes, enhancing diagnostic precision.
Treatment Options: Thrombocythemia vs Polycythemia
Treatment options for Thrombocythemia focus on reducing platelet count and preventing clot formation, often involving low-dose aspirin and myelosuppressive agents such as hydroxyurea. Polycythemia treatment primarily aims to lower red blood cell mass through phlebotomy and cytoreductive therapy, including hydroxyurea or interferon-alpha, to reduce blood viscosity and thrombosis risk. Both conditions require careful monitoring, but Thrombocythemia management targets platelet control, while Polycythemia emphasizes hematocrit reduction.
Complications and Risks: Similarities and Differences
Thrombocythemia and polycythemia both increase the risk of thrombosis, but thrombocythemia primarily causes excessive platelet production leading to clotting or bleeding complications, whereas polycythemia elevates red blood cell mass, increasing blood viscosity and the risk of stroke or myocardial infarction. Both diseases can lead to similar thrombotic events, yet polycythemia patients are more prone to hyperviscosity symptoms such as headaches and dizziness, while thrombocythemia often presents with microvascular disturbances like erythromelalgia. Monitoring for hemorrhagic complications is crucial in thrombocythemia due to platelet dysfunction, contrasting with polycythemia where anticoagulation and phlebotomy mainly address thrombotic risk.
Prognosis and Management: Choosing the Right Approach
Thrombocythemia and polycythemia require distinct management strategies due to differing risks of thrombosis and hemorrhage, with thrombocythemia primarily demanding platelet-lowering therapies such as hydroxyurea or anagrelide. Prognosis in thrombocythemia generally involves a lower risk of transformation to myelofibrosis or acute leukemia compared to polycythemia vera, which necessitates more aggressive control of hematocrit and iron levels. Tailoring treatment based on risk stratification ensures improved patient outcomes and minimizes complications related to blood hyperviscosity and clot formation.
Thrombocythemia and Polycythemia Infographic
 libterm.com
libterm.com