Herpetic whitlow is a painful viral infection caused by the herpes simplex virus, typically affecting the fingers or thumbs with blisters and swelling. Prompt recognition and treatment can prevent complications and reduce discomfort. Discover more about causes, symptoms, and effective management strategies in the rest of this article.
Table of Comparison
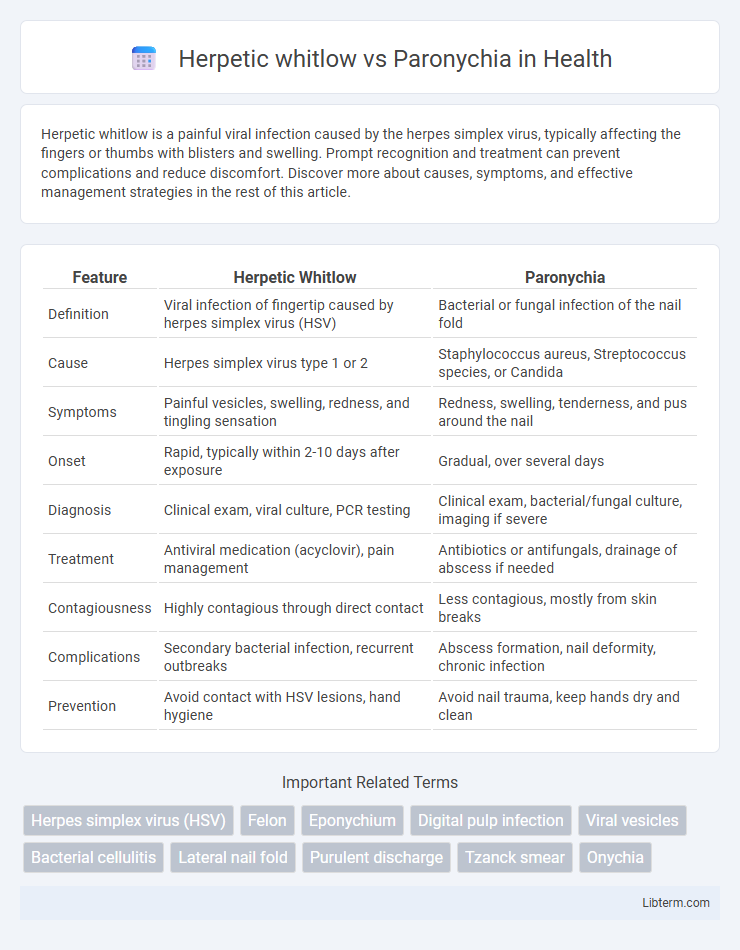
| Feature | Herpetic Whitlow | Paronychia |
|---|---|---|
| Definition | Viral infection of fingertip caused by herpes simplex virus (HSV) | Bacterial or fungal infection of the nail fold |
| Cause | Herpes simplex virus type 1 or 2 | Staphylococcus aureus, Streptococcus species, or Candida |
| Symptoms | Painful vesicles, swelling, redness, and tingling sensation | Redness, swelling, tenderness, and pus around the nail |
| Onset | Rapid, typically within 2-10 days after exposure | Gradual, over several days |
| Diagnosis | Clinical exam, viral culture, PCR testing | Clinical exam, bacterial/fungal culture, imaging if severe |
| Treatment | Antiviral medication (acyclovir), pain management | Antibiotics or antifungals, drainage of abscess if needed |
| Contagiousness | Highly contagious through direct contact | Less contagious, mostly from skin breaks |
| Complications | Secondary bacterial infection, recurrent outbreaks | Abscess formation, nail deformity, chronic infection |
| Prevention | Avoid contact with HSV lesions, hand hygiene | Avoid nail trauma, keep hands dry and clean |
Introduction to Herpetic Whitlow and Paronychia
Herpetic whitlow is a painful viral infection caused by the herpes simplex virus, characterized by swollen, red lesions typically found on the fingers or around the nails. Paronychia is a bacterial or fungal infection affecting the skin around the nail fold, leading to redness, swelling, and pus-filled abscesses. Both conditions cause inflammation near the nail but differ in etiology, treatment, and clinical presentation.
Definition and Causes
Herpetic whitlow is a painful viral infection of the fingers caused by the herpes simplex virus (HSV-1 or HSV-2), characterized by vesicular lesions and swelling, commonly affecting healthcare workers and children. Paronychia is a bacterial or fungal infection of the skin around the fingernail, often caused by Staphylococcus aureus or Candida species, resulting from nail trauma, poor hygiene, or chronic exposure to moisture. Understanding the distinct etiologies--viral for herpetic whitlow and bacterial/fungal for paronychia--guides appropriate diagnosis and treatment.
Epidemiology and Risk Factors
Herpetic whitlow primarily affects healthcare workers and children, with epidemiology linked to exposure to herpes simplex virus types 1 and 2, particularly among those with frequent contact to oral secretions. Paronychia is more common in adults and is frequently associated with occupations involving repeated trauma or exposure to moisture, such as bartenders and dishwashers, with bacterial infection by Staphylococcus aureus being the predominant cause. Both conditions have risk factors related to skin barrier disruption but differ in their infectious agents and demographic prevalence.
Clinical Presentation
Herpetic whitlow presents with grouped vesicular lesions on an erythematous base, typically causing intense pain and localized swelling on the fingers, accompanied by fever and lymphadenopathy in some cases. Paronychia is characterized by erythema, swelling, and tenderness around the nail fold, often with purulent discharge and gradual onset, frequently linked to bacterial infection such as Staphylococcus aureus. Distinguishing features include the presence of vesicles in herpetic whitlow versus abscess formation and pus in acute paronychia.
Pathophysiology
Herpetic whitlow is caused by the herpes simplex virus (HSV) infecting the distal phalanx through breaks in the skin, resulting in vesicular lesions and neural inflammation. Paronychia involves bacterial infection, commonly Staphylococcus aureus or Streptococcus species, affecting the nail fold and causing localized abscess formation and inflammation. The viral etiology of herpetic whitlow leads to cytopathic effects in epidermal cells, whereas paronychia stems from bacterial invasion and subsequent immune response in the periungual tissues.
Diagnostic Criteria and Methods
Herpetic whitlow is diagnosed primarily through clinical examination revealing grouped vesicles on an erythematous base, confirmed by viral culture, polymerase chain reaction (PCR), or Tzanck smear showing multinucleated giant cells. Paronychia diagnosis involves clinical evaluation of localized erythema, swelling, and tenderness around the nail fold, supported by bacterial cultures to identify pathogens such as Staphylococcus aureus or Streptococcus species. Imaging like ultrasound can assist in detecting abscess formation in paronychia but is not typically required for herpetic whitlow.
Differential Diagnosis
Herpetic whitlow presents with grouped vesicular lesions on an erythematous base, often causing intense pain and a history of herpes simplex virus exposure, distinguishing it from paronychia, which typically involves localized bacterial infection with pus formation around the nail fold. Paronychia features swelling, erythema, and tenderness around the nail margin, frequently caused by Staphylococcus aureus or Streptococci, without the vesicular eruptions characteristic of herpetic whitlow. Laboratory confirmation via viral culture or PCR for herpes simplex virus supports diagnosis of herpetic whitlow, whereas bacterial cultures and clinical signs guide identification of paronychia.
Treatment Options
Herpetic whitlow treatment primarily involves antiviral medications such as acyclovir or valacyclovir to reduce viral replication and alleviate symptoms. Paronychia treatment depends on its cause; bacterial paronychia often requires oral or topical antibiotics like cephalexin or clindamycin, while fungal cases are treated with antifungal agents such as fluconazole. Incision and drainage may be necessary for abscess formation in bacterial paronychia but are contraindicated in herpetic whitlow to prevent viral spread.
Complications and Prognosis
Herpetic whitlow can lead to complications such as secondary bacterial infection, herpetic gladiatorum in wrestlers, and rarely, herpetic encephalitis in immunocompromised patients. Paronychia complications include abscess formation, chronic infection, and permanent nail deformity if untreated. Prognosis for herpetic whitlow often involves self-limiting viral resolution within 2-3 weeks, while paronychia may require drainage and antibiotics for complete recovery.
Prevention and Patient Education
Effective prevention of herpetic whitlow involves avoiding direct contact with herpetic lesions, using protective gloves in healthcare settings, and practicing good hand hygiene to reduce HSV transmission. For paronychia, minimizing exposure to moisture and irritants, avoiding nail-biting or finger-sucking, and maintaining proper nail care are crucial to prevent bacterial or fungal infections. Educating patients on early symptom recognition and proper wound care promotes timely treatment and minimizes complications for both conditions.
Herpetic whitlow Infographic
 libterm.com
libterm.com