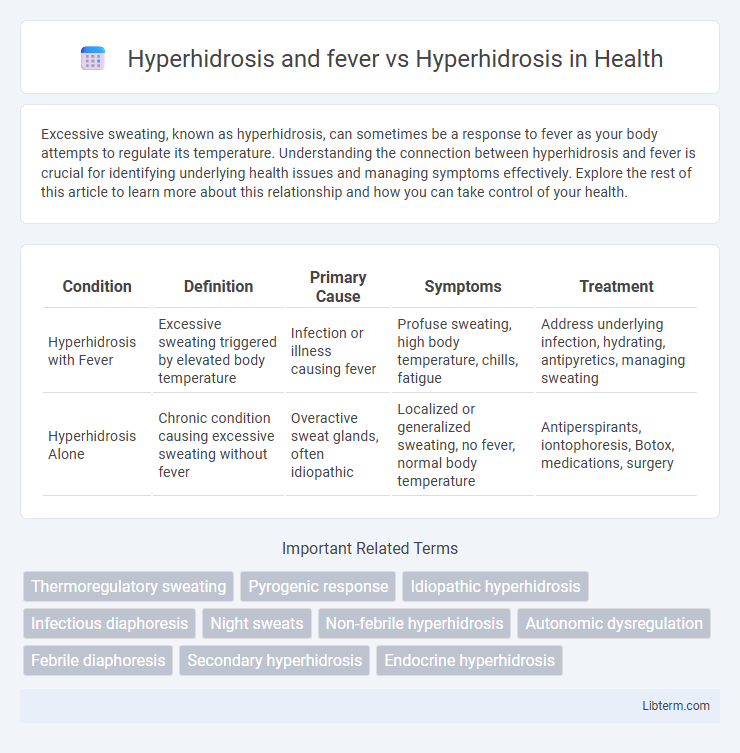
Excessive sweating, known as hyperhidrosis, can sometimes be a response to fever as your body attempts to regulate its temperature. Understanding the connection between hyperhidrosis and fever is crucial for identifying underlying health issues and managing symptoms effectively. Explore the rest of this article to learn more about this relationship and how you can take control of your health.
Table of Comparison
| Condition | Definition | Primary Cause | Symptoms | Treatment |
|---|---|---|---|---|
| Hyperhidrosis with Fever | Excessive sweating triggered by elevated body temperature | Infection or illness causing fever | Profuse sweating, high body temperature, chills, fatigue | Address underlying infection, hydrating, antipyretics, managing sweating |
| Hyperhidrosis Alone | Chronic condition causing excessive sweating without fever | Overactive sweat glands, often idiopathic | Localized or generalized sweating, no fever, normal body temperature | Antiperspirants, iontophoresis, Botox, medications, surgery |
Understanding Hyperhidrosis: Definition and Types
Hyperhidrosis is a medical condition characterized by excessive sweating beyond what is required for temperature regulation, affecting specific areas like palms, feet, or the entire body. Primary hyperhidrosis arises without an underlying cause, often linked to genetic factors, while secondary hyperhidrosis results from medical conditions such as infections, including fever, or hormonal imbalances. Distinguishing between hyperhidrosis and fever-related sweating is crucial, as hyperhidrosis involves persistent sweating independent of body temperature changes, whereas fever-induced sweating occurs as the body attempts to regulate elevated temperature.
Recognizing Fever-Induced Hyperhidrosis
Fever-induced hyperhidrosis often presents as excessive sweating linked to the body's response to infection or illness, differentiating it from primary hyperhidrosis, which is typically unrelated to underlying health conditions. Recognizing fever-induced hyperhidrosis involves monitoring for fever, chills, and systemic symptoms alongside profuse sweating episodes. Accurate identification is critical for appropriate treatment, as managing the underlying fever can reduce hyperhidrosis symptoms.
Key Differences Between Hyperhidrosis and Fever-Related Sweating
Hyperhidrosis causes excessive sweating due to overactive sweat glands without an underlying illness, typically localized and persistent, whereas fever-related sweating results from the body's attempt to regulate abnormal internal temperature during infection or inflammation. In hyperhidrosis, sweating often occurs during rest and is unrelated to heat or exercise, while fever-induced sweating corresponds with spikes in body temperature and usually subsides as the fever breaks. Key differences include the cause, duration, and context of sweating episodes, with hyperhidrosis often requiring targeted treatments and fever-related sweating managed by addressing the underlying infection.
Causes of Primary Hyperhidrosis
Primary hyperhidrosis is caused by overactive sweat glands triggered by the sympathetic nervous system, often without an underlying medical condition, whereas fever-induced sweating results from the body's thermoregulatory response to infection or inflammation. The cause of primary hyperhidrosis remains idiopathic but is believed to involve genetic and neurological factors leading to excessive sweating mainly in the palms, soles, and underarms. Unlike secondary hyperhidrosis associated with fever, primary hyperhidrosis is not linked to systemic illness and typically begins in childhood or adolescence.
Underlying Medical Conditions Linked to Secondary Hyperhidrosis
Secondary hyperhidrosis is often linked to underlying medical conditions such as infections, including fevers caused by viral or bacterial pathogens, thyroid disorders, and certain cancers like lymphoma. These conditions trigger excessive sweating as the body's response to systemic illness or metabolic imbalances. Identifying and treating the root cause is critical for managing secondary hyperhidrosis effectively.
Fever as a Trigger: Pathophysiology and Mechanisms
Hyperhidrosis can be exacerbated by fever, which acts as a key trigger by disrupting normal thermoregulation through hypothalamic set-point elevation. Fever-induced hyperhidrosis involves increased sympathetic nervous system activity causing overactivation of eccrine sweat glands. Understanding this pathophysiology highlights the complex interplay between pyrogenic cytokines and autonomic control in excessive sweating during febrile states.
Diagnostic Criteria: Hyperhidrosis vs. Fever-Induced Sweating
Hyperhidrosis is characterized by excessive, localized sweating without an underlying illness, diagnosed through criteria such as duration of symptoms lasting at least six months, bilateral and symmetric sweating, and absence of fever or systemic infection. Fever-induced sweating, in contrast, is a systemic response to elevated body temperature caused by infections or inflammation, typically involving diffuse sweating accompanied by other symptoms like chills, malaise, and elevated body temperature above 38degC (100.4degF). Diagnostic differentiation hinges on sweat pattern, symptom chronicity, and the presence or absence of systemic signs like fever and infection markers.
Symptom Mapping: Patterns of Sweating in Both Conditions
Hyperhidrosis presents as excessive, localized sweating often affecting palms, soles, and underarms, with no accompanying fever or systemic illness. Fever-related sweating is generalized and typically occurs during febrile episodes as the body attempts to regulate elevated temperature. Symptom mapping reveals hyperhidrosis involves specific sweat pattern triggers unrelated to infection, distinguishing it from fever-induced sweating, which corresponds to systemic inflammatory responses.
Effective Treatment Approaches for Each Condition
Hyperhidrosis treatment focuses on reducing excessive sweating through antiperspirants, Botox injections, oral medications, or sympathectomy surgery, depending on severity and affected areas. Fever-related sweating is managed by addressing the underlying infection or illness with antipyretics like acetaminophen or ibuprofen to reduce body temperature. Tailoring treatment to the root cause ensures effective symptom control and patient comfort for both hyperhidrosis and fever.
When to Seek Medical Advice: Red Flags and Next Steps
Persistent hyperhidrosis accompanied by fever may indicate an underlying infection or systemic condition requiring prompt medical evaluation. Seek medical advice if excessive sweating is sudden, severe, or associated with unexplained weight loss, night sweats, or signs of infection such as chills or fatigue. Early diagnosis and treatment are critical to address potentially serious causes and improve patient outcomes.
Hyperhidrosis and fever Infographic
 libterm.com
libterm.com