Bowel obstruction occurs when the intestines are partially or completely blocked, preventing the normal passage of contents and causing severe abdominal pain, bloating, and vomiting. Timely diagnosis and treatment are crucial to avoid complications such as tissue death or infection. Discover more about the causes, symptoms, and treatment options in the rest of the article.
Table of Comparison
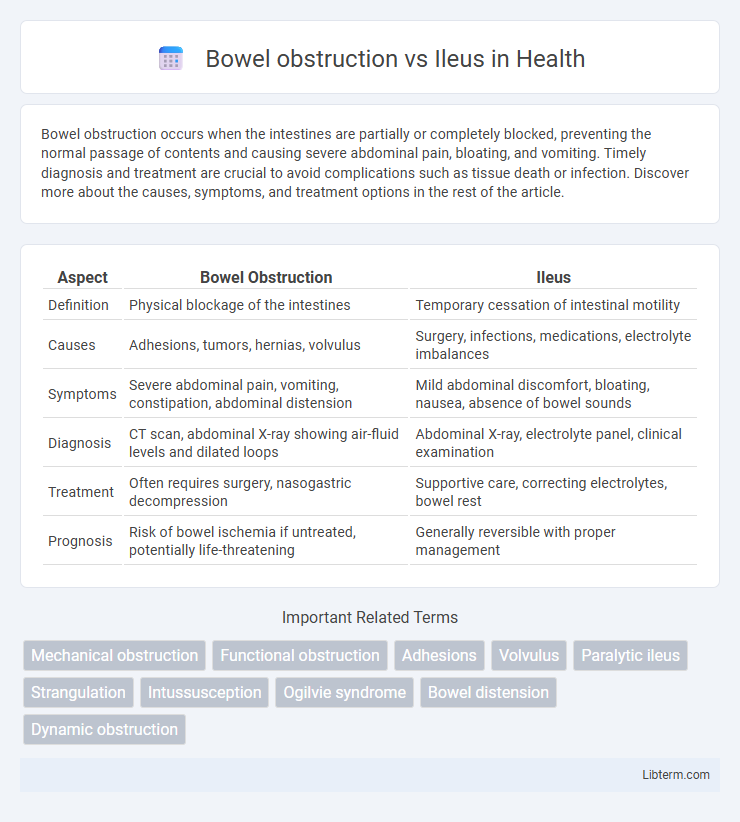
| Aspect | Bowel Obstruction | Ileus |
|---|---|---|
| Definition | Physical blockage of the intestines | Temporary cessation of intestinal motility |
| Causes | Adhesions, tumors, hernias, volvulus | Surgery, infections, medications, electrolyte imbalances |
| Symptoms | Severe abdominal pain, vomiting, constipation, abdominal distension | Mild abdominal discomfort, bloating, nausea, absence of bowel sounds |
| Diagnosis | CT scan, abdominal X-ray showing air-fluid levels and dilated loops | Abdominal X-ray, electrolyte panel, clinical examination |
| Treatment | Often requires surgery, nasogastric decompression | Supportive care, correcting electrolytes, bowel rest |
| Prognosis | Risk of bowel ischemia if untreated, potentially life-threatening | Generally reversible with proper management |
Understanding Bowel Obstruction vs Ileus
Bowel obstruction involves a physical blockage in the intestines preventing normal passage of contents, often caused by adhesions, hernias, or tumors. Ileus refers to a temporary impairment of intestinal motility without a mechanical blockage, commonly resulting from surgery, infection, or medications. Differentiating between bowel obstruction and ileus is crucial for treatment decisions, as obstructions may require surgical intervention while ileus is often managed conservatively.
Definitions: Bowel Obstruction and Ileus
Bowel obstruction is a mechanical blockage preventing the normal passage of intestinal contents due to causes like tumors, adhesions, or hernias, leading to severe abdominal pain and distention. Ileus refers to a functional impairment of intestinal motility without a physical blockage, commonly resulting from surgery, infections, or electrolyte imbalances that disrupt peristalsis. Differentiating bowel obstruction from ileus is crucial for diagnosis and treatment, as obstruction may require surgical intervention while ileus often resolves with supportive care.
Causes of Bowel Obstruction
Bowel obstruction is primarily caused by mechanical factors such as adhesions, hernias, tumors, or strictures that physically block the intestinal lumen, contrasting with ileus, which results from impaired motility without mechanical blockage. Adhesions, often resulting from previous surgeries, account for approximately 60-70% of small bowel obstructions, while hernias contribute around 10-20%. Tumors and inflammatory diseases like Crohn's can also cause partial or complete obstruction, leading to symptoms such as abdominal pain, vomiting, and distension.
Causes of Ileus
Ileus primarily occurs due to disruptions in the normal propulsive ability of the gastrointestinal tract often caused by abdominal surgery, infections such as peritonitis, or metabolic imbalances like hypokalemia. Other common causes include medications that affect bowel motility, including opioids and anticholinergics, as well as systemic illnesses such as sepsis or pancreatitis. Unlike mechanical bowel obstruction, ileus results from a functional impairment rather than a physical blockage.
Symptoms: Comparing Clinical Presentation
Bowel obstruction typically presents with severe abdominal pain, bloating, vomiting, and inability to pass gas or stool, whereas ileus often manifests as mild abdominal discomfort, distension, and reduced or absent bowel sounds without severe pain. In bowel obstruction, symptoms usually develop suddenly and are more intense, reflecting mechanical blockage, while ileus symptoms progress gradually due to temporary paralysis of intestinal motility. Both conditions cause abdominal distension and nausea, but the presence of high-pitched bowel sounds is more characteristic of obstruction, contrasting with the hypoactive or absent bowel sounds seen in ileus.
Diagnostic Approaches and Imaging
Diagnostic approaches for bowel obstruction primarily include abdominal X-rays, which reveal air-fluid levels and dilated bowel loops, while CT scans provide detailed visualization of the obstruction site, cause, and severity. In contrast, ileus diagnosis relies on clinical evaluation and imaging such as abdominal X-rays showing diffuse bowel dilation without a clear mechanical blockage; CT scans help exclude mechanical obstruction and identify underlying causes like inflammation or metabolic disturbances. Ultrasound and fluoroscopy may also aid in distinguishing between mechanical obstruction and ileus, guiding targeted treatment strategies.
Key Differences in Pathophysiology
Bowel obstruction involves a physical blockage of the intestinal lumen, preventing normal passage of contents and leading to increased intraluminal pressure and compromised blood flow. Ileus is characterized by a functional impairment of intestinal motility without a mechanical blockage, caused by disrupted neural or muscular activity in the bowel wall. The primary pathophysiological distinction lies in obstruction causing mechanical interruption, while ileus results from neurogenic or myogenic failure to coordinate peristalsis.
Treatment Strategies: Obstruction vs Ileus
Treatment strategies for bowel obstruction primarily involve surgical intervention to remove or bypass the mechanical blockage, alongside decompression with a nasogastric tube and intravenous fluids to stabilize the patient. In contrast, ileus management focuses on supportive care, including bowel rest, electrolyte correction, and minimizing opioid use to promote the return of normal bowel motility without surgical intervention. Both conditions require careful monitoring for complications like ischemia or perforation, but the definitive treatment differs significantly based on the presence or absence of an anatomical blockage.
Prognosis and Potential Complications
Bowel obstruction typically presents a higher risk of complications such as bowel ischemia, perforation, and sepsis, significantly impacting prognosis if not promptly treated. Ileus often resolves with conservative management, but prolonged cases can lead to electrolyte imbalances, aspiration pneumonia, and increased hospital stay. Early diagnosis and appropriate intervention remain critical factors in improving outcomes for both conditions.
Prevention and Patient Management Tips
Bowel obstruction prevention primarily involves early detection of risk factors such as prior abdominal surgeries, hernias, and inflammatory bowel disease, alongside maintaining a high-fiber diet and adequate hydration to support regular bowel function. Management of bowel obstruction includes timely imaging studies like CT scans, nasogastric decompression, and surgical consultation to avoid complications such as ischemia or perforation, while ileus prevention focuses on minimizing opioid use, promoting early mobilization, and ensuring electrolyte balance. Both conditions benefit from patient education on symptom recognition, adherence to prescribed therapies, and prompt medical evaluation to reduce morbidity and improve outcomes.
Bowel obstruction Infographic
 libterm.com
libterm.com