Respiratory acidosis occurs when the lungs cannot remove enough carbon dioxide, leading to increased blood acidity and disrupted pH balance. This condition often results from chronic respiratory diseases, impaired lung function, or hypoventilation, requiring prompt medical evaluation to prevent severe complications. Explore the rest of this article to understand symptoms, causes, and effective treatment options for respiratory acidosis.
Table of Comparison
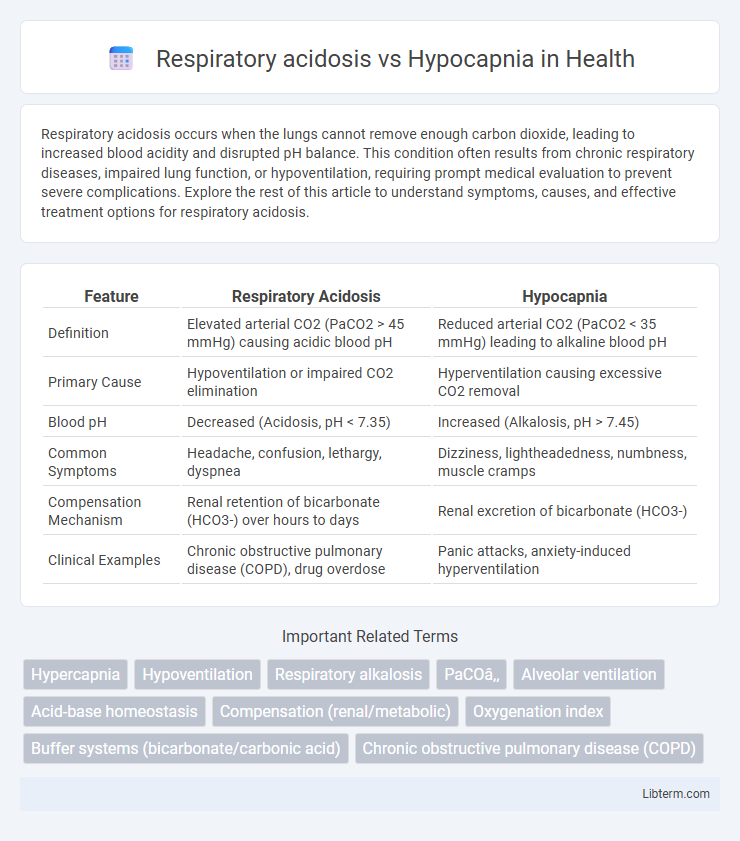
| Feature | Respiratory Acidosis | Hypocapnia |
|---|---|---|
| Definition | Elevated arterial CO2 (PaCO2 > 45 mmHg) causing acidic blood pH | Reduced arterial CO2 (PaCO2 < 35 mmHg) leading to alkaline blood pH |
| Primary Cause | Hypoventilation or impaired CO2 elimination | Hyperventilation causing excessive CO2 removal |
| Blood pH | Decreased (Acidosis, pH < 7.35) | Increased (Alkalosis, pH > 7.45) |
| Common Symptoms | Headache, confusion, lethargy, dyspnea | Dizziness, lightheadedness, numbness, muscle cramps |
| Compensation Mechanism | Renal retention of bicarbonate (HCO3-) over hours to days | Renal excretion of bicarbonate (HCO3-) |
| Clinical Examples | Chronic obstructive pulmonary disease (COPD), drug overdose | Panic attacks, anxiety-induced hyperventilation |
Understanding Respiratory Acidosis
Respiratory acidosis occurs when impaired lung function causes hypoventilation, leading to elevated arterial carbon dioxide (PaCO2) levels and decreased blood pH. This condition is often seen in chronic obstructive pulmonary disease (COPD), neuromuscular disorders, or severe asthma exacerbations, resulting in CO2 retention and acid-base imbalance. Effective management requires addressing the underlying cause and improving ventilation to restore normal PaCO2 and pH levels.
What Is Hypocapnia?
Hypocapnia is a condition characterized by reduced carbon dioxide (CO2) levels in the blood, typically resulting from hyperventilation or increased respiratory rate. Unlike respiratory acidosis, which involves elevated CO2 and decreased blood pH, hypocapnia leads to respiratory alkalosis due to excessive CO2 elimination. Understanding the difference between hypocapnia and respiratory acidosis is essential for accurate diagnosis and treatment in respiratory and metabolic disorders.
Causes of Respiratory Acidosis
Respiratory acidosis results from hypoventilation causing elevated arterial carbon dioxide (PaCO2) levels, commonly due to chronic obstructive pulmonary disease (COPD), respiratory muscle weakness, or central nervous system depression from drugs or trauma. Hypocapnia, by contrast, involves reduced PaCO2 from hyperventilation and often occurs in anxiety or metabolic acidosis compensation. Understanding the causes of respiratory acidosis is critical for identifying impaired ventilation and ensuring timely intervention to restore acid-base balance.
Common Triggers of Hypocapnia
Hypocapnia commonly results from hyperventilation due to anxiety, fever, sepsis, or pulmonary embolism, leading to decreased partial pressure of carbon dioxide (PaCO2) in the blood. Unlike respiratory acidosis, which is characterized by elevated PaCO2 from hypoventilation or impaired gas exchange, hypocapnia reflects excessive CO2 elimination and respiratory alkalosis. Recognizing these triggers is crucial for differential diagnosis and appropriate management of acid-base imbalances.
Clinical Manifestations and Symptoms
Respiratory acidosis presents with symptoms such as headache, confusion, lethargy, and shortness of breath due to elevated arterial carbon dioxide (PaCO2) levels causing acid-base imbalance. In contrast, hypocapnia, characterized by decreased PaCO2, leads to symptoms like dizziness, lightheadedness, paresthesia, and muscle cramps resulting from respiratory alkalosis and cerebral vasoconstriction. Clinical manifestations of respiratory acidosis often indicate hypoventilation and CO2 retention, while hypocapnia symptoms reflect hyperventilation and reduced cerebral blood flow.
Diagnostic Markers: Blood Gas Analysis
Respiratory acidosis is characterized by elevated partial pressure of carbon dioxide (PaCO2) above 45 mmHg and decreased blood pH below 7.35 due to hypoventilation. Hypocapnia demonstrates reduced PaCO2 levels below 35 mmHg, often with a compensatory increase in blood pH indicating respiratory alkalosis. Blood gas analysis, measuring PaCO2, pH, and bicarbonate (HCO3-) concentrations, is essential for differentiating respiratory acidosis from hypocapnia and guiding appropriate clinical interventions.
Pathophysiological Differences
Respiratory acidosis is characterized by elevated arterial CO2 levels due to hypoventilation, causing a primary increase in PaCO2 and subsequent decrease in blood pH. Hypocapnia involves reduced PaCO2 from hyperventilation, leading to respiratory alkalosis with increased blood pH. The pathophysiological difference lies in CO2 retention versus CO2 depletion, directly affecting acid-base homeostasis and respiratory drive regulation.
Treatment Approaches and Management
Respiratory acidosis treatment centers on improving alveolar ventilation through methods such as mechanical ventilation or bronchodilators to reduce elevated arterial carbon dioxide levels. Hypocapnia management involves addressing underlying causes like hyperventilation syndrome with anxiolytics or controlled breathing techniques to restore normal pCO2 levels. Monitoring arterial blood gases is crucial in both conditions to guide therapy and prevent complications associated with imbalanced carbon dioxide homeostasis.
Potential Complications and Risks
Respiratory acidosis, characterized by elevated carbon dioxide (CO2) levels due to hypoventilation, can lead to complications such as respiratory failure, altered mental status, and arrhythmias. Hypocapnia, resulting from excessive CO2 elimination often caused by hyperventilation, increases the risk of cerebral vasoconstriction, leading to dizziness, syncope, and impaired oxygen delivery to brain tissues. Both conditions can disrupt acid-base balance, necessitating careful monitoring to prevent severe neurological and cardiovascular complications.
Preventive Strategies and Patient Education
Preventive strategies for respiratory acidosis emphasize managing chronic lung diseases through smoking cessation, avoiding respiratory depressants, and ensuring adherence to prescribed treatments like bronchodilators or oxygen therapy. Patient education should focus on recognizing early symptoms such as shortness of breath and confusion, proper use of inhalers, and the importance of regular pulmonary function monitoring. For hypocapnia, teaching patients stress-reduction techniques, controlled breathing exercises, and awareness of hyperventilation triggers helps prevent excessive CO2 loss and maintains acid-base balance.
Respiratory acidosis Infographic
 libterm.com
libterm.com