Necrosis is the premature death of cells in living tissue caused by factors such as infection, toxins, or trauma. This condition disrupts normal cell function and can lead to inflammation and tissue damage if left untreated. Explore the details of necrosis, including its causes, symptoms, and treatment options, to better understand its impact on your health.
Table of Comparison
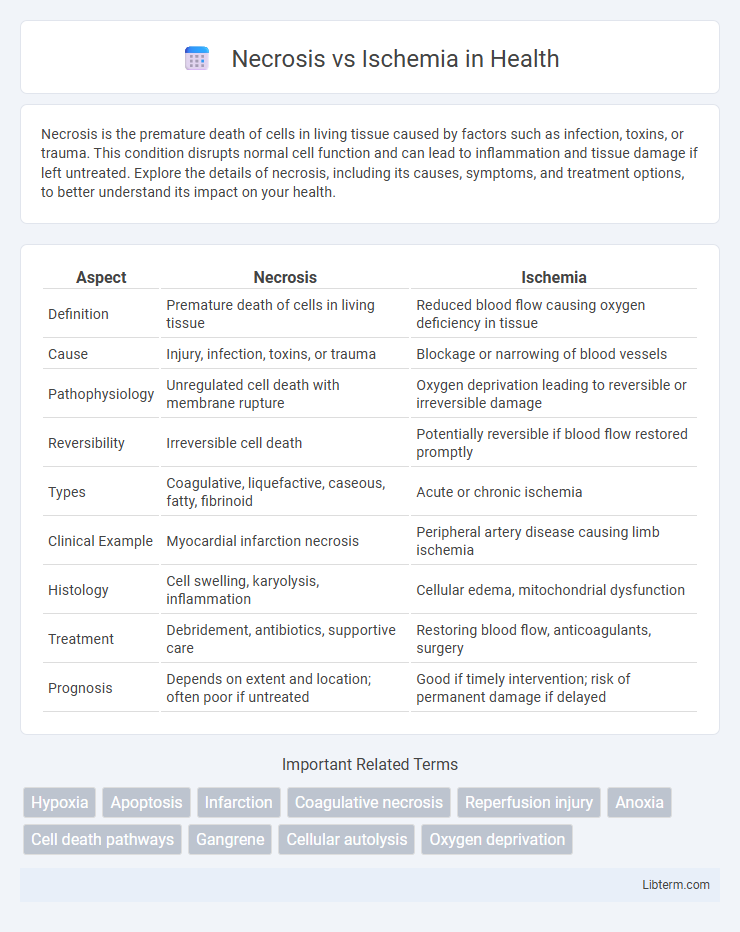
| Aspect | Necrosis | Ischemia |
|---|---|---|
| Definition | Premature death of cells in living tissue | Reduced blood flow causing oxygen deficiency in tissue |
| Cause | Injury, infection, toxins, or trauma | Blockage or narrowing of blood vessels |
| Pathophysiology | Unregulated cell death with membrane rupture | Oxygen deprivation leading to reversible or irreversible damage |
| Reversibility | Irreversible cell death | Potentially reversible if blood flow restored promptly |
| Types | Coagulative, liquefactive, caseous, fatty, fibrinoid | Acute or chronic ischemia |
| Clinical Example | Myocardial infarction necrosis | Peripheral artery disease causing limb ischemia |
| Histology | Cell swelling, karyolysis, inflammation | Cellular edema, mitochondrial dysfunction |
| Treatment | Debridement, antibiotics, supportive care | Restoring blood flow, anticoagulants, surgery |
| Prognosis | Depends on extent and location; often poor if untreated | Good if timely intervention; risk of permanent damage if delayed |
Introduction to Necrosis and Ischemia
Necrosis is the premature death of cells and tissues caused by factors such as infection, toxins, or trauma, leading to the uncontrolled breakdown of cellular structures. Ischemia refers to the insufficient blood supply to tissues, resulting in a lack of oxygen and nutrients necessary for cell survival, often serving as a primary cause of necrosis. Both conditions critically disrupt cellular metabolism and can lead to significant tissue damage if not promptly addressed.
Defining Necrosis: Causes and Characteristics
Necrosis is the irreversible death of cells or tissues caused by factors such as infection, toxins, trauma, or interrupted blood supply. It is characterized by cellular swelling, loss of membrane integrity, enzyme leakage, and inflammation in surrounding tissues. Unlike ischemia, which is the reduced blood flow leading to oxygen deprivation, necrosis signifies the endpoint of sustained cellular injury resulting in tissue breakdown.
Understanding Ischemia: Mechanisms and Triggers
Ischemia occurs when blood flow to tissues is restricted, causing a critical deficiency of oxygen and nutrients essential for cellular survival. This deprivation triggers a cascade of biochemical events, including ATP depletion, ion imbalance, and accumulation of toxic metabolites, which ultimately disrupt cellular functions. Understanding these mechanisms highlights ischemia's role in initiating cell injury distinct from necrosis, which is the irreversible endpoint of severe ischemic damage when cells undergo uncontrolled death.
Key Differences Between Necrosis and Ischemia
Necrosis is the irreversible death of cells or tissues due to injury or disease, whereas ischemia refers to the reduced blood flow causing oxygen deprivation to tissues. Necrosis results in structural cell damage and inflammation, while ischemia primarily causes functional impairment that may lead to necrosis if prolonged. Clinically, ischemia is often reversible with timely intervention, but necrosis indicates permanent tissue loss requiring more extensive medical treatment.
Common Causes of Necrosis
Necrosis commonly results from factors such as infection, toxin exposure, trauma, and impaired blood supply leading to cell death in affected tissues. Unlike ischemia, which specifically refers to restricted blood flow causing oxygen deprivation, necrosis encompasses a broader range of pathological processes resulting in uncontrolled cell damage. Understanding these causes is essential for diagnosing and treating tissue injury effectively.
Typical Triggers of Ischemia
Ischemia typically results from obstruction of blood flow due to conditions such as atherosclerosis, thrombosis, or embolism, which reduce oxygen supply to tissues. Coronary artery disease is a common cause leading to myocardial ischemia, while cerebrovascular obstruction often triggers ischemic stroke. These vascular events deprive cells of essential nutrients and oxygen, initiating the cascade towards tissue injury and potential necrosis.
Clinical Manifestations of Necrosis Versus Ischemia
Necrosis presents clinically with localized tissue death, often accompanied by severe pain, swelling, and discoloration, sometimes progressing to gangrene or systemic signs of infection like fever and sepsis. Ischemia typically manifests as pain due to inadequate blood supply, pallor, diminished pulses, and functional impairment of the affected organ or tissue without immediate cell death. Early ischemic symptoms can be reversible, whereas necrosis indicates irreversible cellular injury and often requires surgical intervention to prevent further complications.
Diagnostic Approaches for Necrosis and Ischemia
Diagnostic approaches for necrosis primarily involve imaging techniques such as MRI and CT scans to identify tissue death and assess the extent of damage. For ischemia, Doppler ultrasound and angiography are commonly used to evaluate blood flow and detect arterial blockages causing insufficient oxygen supply. Biomarker analysis, including serum lactate levels and troponin tests, aids in distinguishing ischemic injury from necrotic tissue damage.
Treatment Strategies: Necrosis vs Ischemia
Treatment strategies for necrosis focus on removing dead tissue through surgical debridement and preventing infection with antibiotics, while ischemia management prioritizes restoring blood flow via revascularization techniques such as angioplasty or bypass surgery. Necrosis often necessitates supportive care to promote healing and manage complications, whereas ischemia therapy involves controlling underlying causes like atherosclerosis and improving oxygen delivery to affected tissues. Timely intervention in ischemia can prevent progression to necrosis, emphasizing the importance of early diagnosis and tailored vascular treatments.
Preventive Measures and Prognosis
Preventive measures for necrosis and ischemia primarily involve maintaining adequate blood flow and oxygen delivery to tissues through managing risk factors such as hypertension, diabetes, and atherosclerosis. Early detection and treatment of ischemic events can significantly improve prognosis by preventing irreversible tissue damage and progression to necrosis. Prognosis depends on the extent and duration of ischemia; timely intervention often leads to tissue recovery, whereas delayed treatment results in necrosis with potential for permanent functional impairment.
Necrosis Infographic
 libterm.com
libterm.com