Leukoplakia is a condition characterized by white patches on the mucous membranes of the mouth, often considered a precancerous lesion with the potential to develop into oral cancer. Understanding the risk factors, early signs, and treatment options is crucial for preventing malignant transformation and ensuring your oral health. Explore the rest of the article to learn how to recognize leukoplakia and reduce your risk of oral cancer.
Table of Comparison
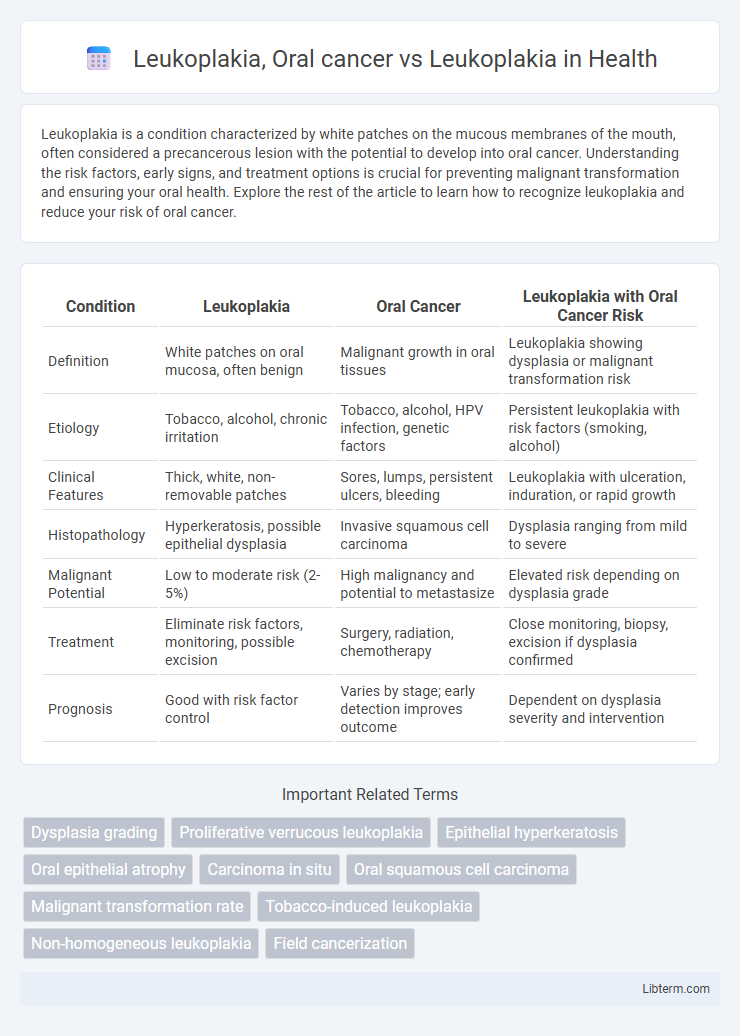
| Condition | Leukoplakia | Oral Cancer | Leukoplakia with Oral Cancer Risk |
|---|---|---|---|
| Definition | White patches on oral mucosa, often benign | Malignant growth in oral tissues | Leukoplakia showing dysplasia or malignant transformation risk |
| Etiology | Tobacco, alcohol, chronic irritation | Tobacco, alcohol, HPV infection, genetic factors | Persistent leukoplakia with risk factors (smoking, alcohol) |
| Clinical Features | Thick, white, non-removable patches | Sores, lumps, persistent ulcers, bleeding | Leukoplakia with ulceration, induration, or rapid growth |
| Histopathology | Hyperkeratosis, possible epithelial dysplasia | Invasive squamous cell carcinoma | Dysplasia ranging from mild to severe |
| Malignant Potential | Low to moderate risk (2-5%) | High malignancy and potential to metastasize | Elevated risk depending on dysplasia grade |
| Treatment | Eliminate risk factors, monitoring, possible excision | Surgery, radiation, chemotherapy | Close monitoring, biopsy, excision if dysplasia confirmed |
| Prognosis | Good with risk factor control | Varies by stage; early detection improves outcome | Dependent on dysplasia severity and intervention |
Understanding Leukoplakia: Definition and Causes
Leukoplakia is a condition characterized by thick, white patches on the mucous membranes of the oral cavity, primarily caused by chronic irritation from tobacco use, alcohol consumption, or friction from dental appliances. While leukoplakia itself is a benign lesion, it is considered a precancerous condition with a risk of progressing to oral cancer, particularly when dysplastic changes are present in the epithelial tissue. Early diagnosis and monitoring of leukoplakia are crucial for preventing malignant transformation and managing oral health effectively.
Oral Cancer vs Leukoplakia: Key Differences
Oral cancer and leukoplakia differ significantly in their pathology; oral cancer is a malignant tumor arising from the squamous cells lining the mouth, whereas leukoplakia presents as white patches or plaques that are predominantly benign but may have precancerous potential. Leukoplakia lesions require careful monitoring due to their risk of malignant transformation, especially when dysplasia is present, while oral cancer demands immediate and aggressive treatment due to its invasive nature and potential for metastasis. The primary diagnostic tools include biopsy for histopathological analysis and imaging studies to assess tumor extent in oral cancer, contrasting with clinical examination and longitudinal follow-up for leukoplakia management.
Early Signs and Symptoms to Watch For
Leukoplakia presents as white or gray patches on the tongue, gums, or inside of the cheek, often painless but potentially precancerous, requiring careful monitoring. Early signs of oral cancer include persistent sores, red or white patches, bleeding, or lumps in the mouth that do not heal within two weeks. Detecting these symptoms promptly enables early diagnosis and intervention, significantly improving treatment outcomes and prognosis.
Risk Factors Associated with Leukoplakia and Oral Cancer
Leukoplakia is primarily linked to tobacco use, chronic irritation, and alcohol consumption, which are also significant risk factors for oral cancer. Persistent leukoplakia lesions, especially those exhibiting dysplasia, can progress to oral squamous cell carcinoma, highlighting the critical need for early detection and monitoring. Human papillomavirus (HPV) infection and poor oral hygiene further contribute to the increased risk of malignant transformation in patients with leukoplakia.
Diagnostic Methods for Leukoplakia and Oral Cancer
Leukoplakia diagnosis primarily relies on clinical examination followed by biopsy to confirm epithelial dysplasia or carcinoma in situ, using histopathological analysis as the gold standard. Oral cancer diagnosis incorporates imaging techniques such as MRI and CT scans alongside tissue biopsy to assess tumor extent and metastasis. Adjunctive diagnostic tools like toluidine blue staining, autofluorescence, and brush biopsy enhance early detection and differentiation between benign leukoplakia and malignant oral lesions.
Histopathological Features: Leukoplakia vs Oral Cancer
Leukoplakia histopathologically presents with hyperkeratosis, epithelial hyperplasia, or varying degrees of dysplasia without invasion of the basement membrane. In contrast, oral cancer, particularly squamous cell carcinoma, exhibits disruption of the basement membrane with malignant epithelial cells invading the underlying connective tissue. The presence of severe dysplasia, cellular atypia, and invasion are key histopathological criteria distinguishing oral cancer from leukoplakia.
Progression: When Leukoplakia Turns Malignant
Leukoplakia is a white patch in the oral cavity with potential for malignant transformation, making early detection crucial for preventing oral cancer. Studies indicate that approximately 1-20% of leukoplakia cases progress to oral squamous cell carcinoma, with factors such as dysplasia severity, lesion size, and tobacco use influencing this risk. Regular monitoring and biopsy of suspicious leukoplakia lesions help assess dysplastic changes and guide timely intervention to halt progression to oral cancer.
Treatment Options for Leukoplakia and Oral Cancer
Treatment options for leukoplakia primarily involve monitoring small, non-dysplastic lesions with regular oral examinations and eliminating risk factors such as tobacco and alcohol use. In cases of leukoplakia with dysplasia or high malignant potential, surgical excision, laser therapy, or cryotherapy are recommended to prevent progression to oral cancer. Oral cancer treatment typically requires a multidisciplinary approach including surgery, radiation therapy, and chemotherapy, depending on tumor stage and location, with targeted therapies and immunotherapy emerging as options for advanced cases.
Prevention Strategies and Lifestyle Modifications
Effective prevention strategies for leukoplakia and oral cancer emphasize eliminating tobacco use, reducing alcohol consumption, and maintaining excellent oral hygiene to minimize mucosal irritation. Regular dental check-ups and early biopsies of suspicious lesions enhance early detection and timely intervention, reducing malignant transformation risks. Nutritional improvements, such as a diet rich in antioxidants and vitamins A, C, and E, support mucosal health and may lower oral leukoplakia progression to oral cancer.
Prognosis and Long-term Management Strategies
Leukoplakia, a potentially precancerous oral lesion, requires vigilant monitoring due to its risk of malignant transformation into oral cancer. Prognosis significantly worsens once leukoplakia progresses to oral cancer, with survival rates dropping based on cancer stage and metastasis. Long-term management involves regular clinical evaluation, biopsy for dysplasia assessment, lifestyle modifications like tobacco cessation, and possibly surgical excision or laser therapy to mitigate the risk of malignancy.
Leukoplakia, Oral cancer Infographic
 libterm.com
libterm.com