Stroke occurs when blood flow to the brain is interrupted, causing brain cells to die rapidly and leading to serious neurological impairments. Recognizing symptoms early and seeking immediate medical treatment can significantly improve recovery and reduce long-term damage. Discover more about stroke prevention, diagnosis, and treatment options to protect Your brain health in the full article.
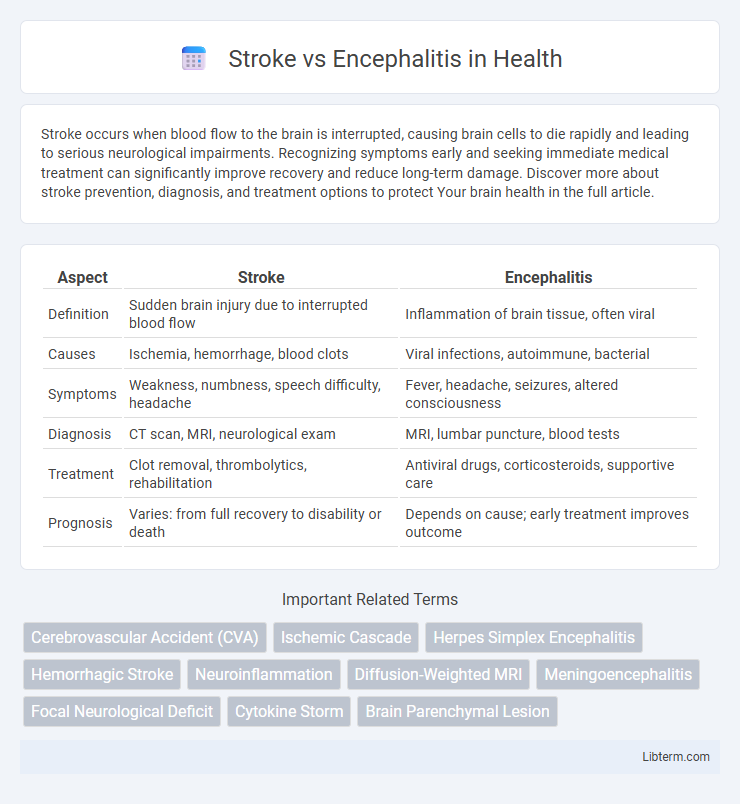
Table of Comparison
| Aspect | Stroke | Encephalitis |
|---|---|---|
| Definition | Sudden brain injury due to interrupted blood flow | Inflammation of brain tissue, often viral |
| Causes | Ischemia, hemorrhage, blood clots | Viral infections, autoimmune, bacterial |
| Symptoms | Weakness, numbness, speech difficulty, headache | Fever, headache, seizures, altered consciousness |
| Diagnosis | CT scan, MRI, neurological exam | MRI, lumbar puncture, blood tests |
| Treatment | Clot removal, thrombolytics, rehabilitation | Antiviral drugs, corticosteroids, supportive care |
| Prognosis | Varies: from full recovery to disability or death | Depends on cause; early treatment improves outcome |
Introduction to Stroke and Encephalitis
Stroke occurs due to impaired blood flow to the brain, resulting in sudden neurological deficits and potential brain damage, while encephalitis is an inflammation of the brain tissue typically caused by viral infections or autoimmune responses. Both conditions present with altered mental status and neurological symptoms, but stroke primarily involves vascular blockage or hemorrhage, whereas encephalitis involves infection-driven inflammation. Rapid diagnosis using imaging techniques like MRI and specific laboratory tests is crucial to differentiate and manage these distinct but severe neurological disorders effectively.
Defining Stroke: Causes and Mechanisms
Stroke is caused by interrupted blood flow to the brain, primarily due to ischemia from a blood clot or hemorrhage from a ruptured vessel. This disruption results in oxygen deprivation and subsequent neuronal damage, leading to sudden neurological deficits. Key mechanisms include arterial blockage, vessel rupture, and impaired cerebral perfusion, which differentiate it from inflammatory brain conditions like encephalitis.
Understanding Encephalitis: Triggers and Pathology
Encephalitis is an inflammatory brain condition primarily triggered by viral infections such as herpes simplex virus, autoimmune responses, or less commonly, bacterial or fungal agents. This inflammation leads to brain tissue swelling, neuronal damage, and altered neurological function, differentiating it pathologically from stroke, which involves sudden ischemia or hemorrhage causing localized brain damage. Understanding the triggers and pathological mechanisms helps in accurate diagnosis and targeted treatment distinguishing encephalitis from cerebrovascular events.
Key Differences Between Stroke and Encephalitis
Stroke primarily results from interrupted blood flow to the brain, causing sudden neurological deficits, while encephalitis is an inflammation of brain tissue typically caused by viral infections, leading to symptoms like fever, headache, and altered consciousness. Stroke symptoms often present abruptly with unilateral weakness, speech difficulties, or visual disturbances, whereas encephalitis develops more gradually, marked by systemic signs of infection and cognitive impairment. Diagnostic imaging such as CT or MRI reveals ischemic or hemorrhagic lesions in stroke, contrasted with diffuse or focal brain inflammation seen in encephalitis through MRI and cerebrospinal fluid analysis.
Common Symptoms: Stroke vs. Encephalitis
Stroke commonly presents with sudden numbness or weakness on one side of the body, confusion, difficulty speaking, and vision problems, indicating impaired blood flow to the brain. Encephalitis symptoms include fever, headache, altered mental status, seizures, and sensitivity to light, reflecting brain inflammation. Both conditions require immediate medical evaluation but can be differentiated by the presence of fever and infection signs in encephalitis versus the abrupt neurological deficits typical of stroke.
Diagnostic Approaches for Both Conditions
Stroke diagnosis relies heavily on neuroimaging techniques such as computed tomography (CT) and magnetic resonance imaging (MRI) to identify ischemic or hemorrhagic regions in the brain. Encephalitis diagnosis involves cerebrospinal fluid (CSF) analysis through lumbar puncture, alongside MRI to detect inflammation and viral or autoimmune markers. Electroencephalography (EEG) can assist in differentiating encephalitis by identifying characteristic brain wave abnormalities not typically present in stroke.
Treatment Options: Stroke vs. Encephalitis
Stroke treatment involves rapid restoration of blood flow through thrombolysis or mechanical thrombectomy for ischemic stroke, while hemorrhagic stroke may require surgical intervention to control bleeding. Encephalitis management focuses on antiviral or antibiotic therapy, depending on the underlying infectious cause, along with supportive care such as corticosteroids to reduce brain inflammation. Rehabilitation therapies, including physical, occupational, and speech therapy, are critical in both conditions to improve neurological function and patient outcomes.
Complications and Long-term Effects
Stroke complications often include paralysis, speech difficulties, and cognitive impairments due to brain tissue damage caused by interrupted blood flow. Encephalitis can lead to seizures, memory loss, and behavioral changes resulting from inflammation and infection of brain tissues. Both conditions may result in long-term neurological deficits, but stroke typically causes localized brain damage while encephalitis often produces more diffuse brain dysfunction.
Prevention Strategies and Risk Factors
Stroke prevention strategies primarily target controlling high blood pressure, managing diabetes, and adopting a healthy lifestyle with regular exercise and a balanced diet to reduce atherosclerosis and clot formation. Encephalitis prevention emphasizes vaccination against viruses such as herpes simplex and arboviruses, along with measures to avoid mosquito bites and reduce exposure to infectious agents. Key risk factors for stroke include hypertension, smoking, atrial fibrillation, and obesity, while encephalitis risk increases with immune suppression, exposure to viral infections, and geographic areas with high vector-borne disease prevalence.
When to Seek Medical Help
Seek immediate medical attention if experiencing sudden weakness, numbness, confusion, difficulty speaking, or severe headache, as these are critical signs of a stroke requiring urgent intervention. Encephalitis symptoms like persistent fever, severe headache, seizures, or altered consciousness also demand prompt emergency evaluation to prevent long-term neurological damage. Early diagnosis and treatment in both stroke and encephalitis significantly improve patient outcomes and reduce the risk of permanent disability.
Stroke Infographic
 libterm.com
libterm.com