Menopause often triggers hormonal changes that can lead to hyperhidrosis, characterized by excessive sweating, especially during hot flashes and night sweats. Managing these symptoms requires targeted approaches including lifestyle adjustments and medical treatments to restore your comfort. Discover effective strategies to control hyperhidrosis during menopause in the rest of this article.
Table of Comparison
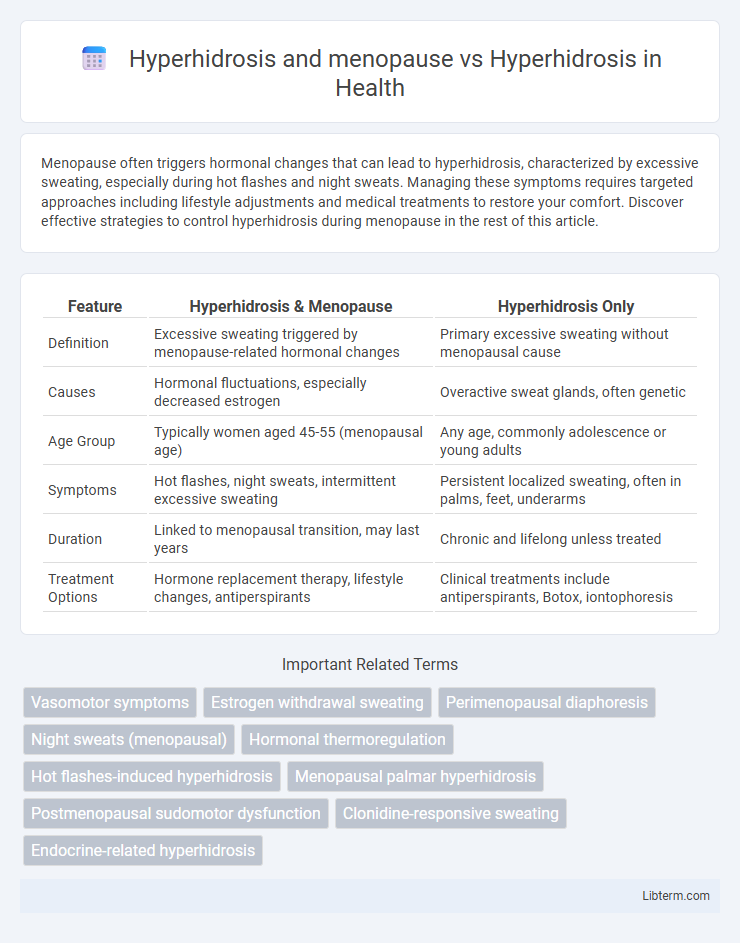
| Feature | Hyperhidrosis & Menopause | Hyperhidrosis Only |
|---|---|---|
| Definition | Excessive sweating triggered by menopause-related hormonal changes | Primary excessive sweating without menopausal cause |
| Causes | Hormonal fluctuations, especially decreased estrogen | Overactive sweat glands, often genetic |
| Age Group | Typically women aged 45-55 (menopausal age) | Any age, commonly adolescence or young adults |
| Symptoms | Hot flashes, night sweats, intermittent excessive sweating | Persistent localized sweating, often in palms, feet, underarms |
| Duration | Linked to menopausal transition, may last years | Chronic and lifelong unless treated |
| Treatment Options | Hormone replacement therapy, lifestyle changes, antiperspirants | Clinical treatments include antiperspirants, Botox, iontophoresis |
Understanding Hyperhidrosis: Overview and Symptoms
Hyperhidrosis is characterized by excessive sweating beyond the body's cooling needs, often affecting palms, feet, underarms, and face, and can be primary or secondary. Menopause-related hyperhidrosis results from hormonal fluctuations, typically involving night sweats and hot flashes linked to estrogen decline. Understanding these distinctions aids in accurate diagnosis and targeted treatments for persistent excessive sweating versus menopause-induced symptoms.
Menopause-Related Hyperhidrosis: Causes and Triggers
Menopause-related hyperhidrosis primarily results from hormonal fluctuations, especially the decline in estrogen levels, which disrupts the body's temperature regulation. Triggers include hot flashes, stress, and changes in the hypothalamus, intensifying excessive sweating episodes during menopause. Understanding these causes helps differentiate menopause-induced hyperhidrosis from other types, aiding targeted treatments.
Primary vs Secondary Hyperhidrosis: Key Differences
Primary hyperhidrosis is a chronic condition characterized by excessive sweating without an underlying cause, often affecting palms, soles, and underarms, while secondary hyperhidrosis results from an underlying medical condition, such as menopause, infections, or endocrine disorders. Menopause-related hyperhidrosis typically presents as a symptom of secondary hyperhidrosis due to hormonal fluctuations causing night sweats and hot flashes. Understanding these distinctions is crucial for effective diagnosis and targeted treatment strategies.
Hormonal Changes in Menopause and Their Role in Excessive Sweating
Hormonal changes during menopause, particularly fluctuations in estrogen and progesterone levels, significantly contribute to the onset of hyperhidrosis by disrupting the body's temperature regulation system. These hormonal shifts stimulate the hypothalamus, triggering excessive sweating episodes commonly known as hot flashes or night sweats in menopausal women. Unlike primary hyperhidrosis, which arises without an underlying cause, menopause-related hyperhidrosis is directly tied to endocrine changes that exacerbate sweat gland activity and impact quality of life.
Diagnostic Approaches: Identifying Hyperhidrosis Types
Differentiating primary hyperhidrosis from secondary hyperhidrosis linked to menopause requires targeted diagnostic approaches, including detailed patient history, symptom pattern analysis, and exclusion of underlying conditions such as hormonal imbalances. Ambulatory sweat tests, like the Minor starch-iodine test, help localize excessive sweating areas, while serum hormone level assessments identify menopausal endocrine changes. Accurate classification enables tailored management strategies addressing either idiopathic nerve hyperactivity or menopause-related sudomotor dysfunction.
Impact on Quality of Life: Menopausal vs General Hyperhidrosis
Hyperhidrosis during menopause often leads to intense, unpredictable night sweats that disrupt sleep and heighten emotional stress, significantly impairing quality of life compared to general hyperhidrosis. General hyperhidrosis usually involves persistent, excessive sweating in specific areas like palms or underarms, causing social anxiety and daily functional limitations. The cyclical hormonal fluctuations in menopause exacerbate sweating episodes, increasing psychological distress and reducing overall well-being more than idiopathic hyperhidrosis.
Treatment Options for Menopausal Hyperhidrosis
Menopausal hyperhidrosis often requires targeted treatment that differs from general hyperhidrosis management due to hormonal fluctuations causing excessive sweating. Effective treatments include hormone replacement therapy (HRT), which helps regulate estrogen levels and reduce sweating episodes, alongside traditional approaches such as antiperspirants containing aluminum chloride, oral medications like clonidine, and lifestyle modifications. Non-hormonal interventions like botulinum toxin injections and cognitive-behavioral therapy offer symptomatic relief when hormonal treatments are contraindicated or insufficient.
Conventional Therapies for Non-Menopausal Hyperhidrosis
Conventional therapies for non-menopausal hyperhidrosis typically include topical antiperspirants containing aluminum chloride, oral anticholinergic medications, and botulinum toxin injections, which effectively reduce excessive sweating by targeting sweat glands. Iontophoresis is often employed as a non-invasive treatment, using electrical currents to temporarily block sweat production, primarily in the hands and feet. In severe cases, surgical interventions such as endoscopic thoracic sympathectomy (ETS) may be considered, although these procedures carry risks and are reserved for refractory hyperhidrosis unresponsive to conservative management.
Lifestyle Modifications for Managing Hyperhidrosis in Menopause
Lifestyle modifications for managing hyperhidrosis during menopause include wearing breathable, moisture-wicking fabrics to enhance comfort and reduce sweating episodes. Incorporating stress-reduction techniques like yoga or meditation can help regulate hormone fluctuations that exacerbate sweating. Staying hydrated and avoiding spicy foods, caffeine, and alcohol may also minimize excessive sweating linked to menopausal hormonal changes.
When to Seek Medical Advice: Recognizing Severe Hyperhidrosis
Severe hyperhidrosis during menopause often involves sudden, intense night sweats and excessive sweating beyond typical hormonal fluctuations, signaling a need for medical evaluation. Hyperhidrosis unrelated to menopause presents as persistent, localized sweating unaffected by temperature or stress, warranting clinical assessment to rule out underlying conditions. Prompt consultation with a healthcare provider ensures accurate diagnosis and tailored treatment for severe hyperhidrosis symptoms, improving quality of life and preventing complications.
Hyperhidrosis and menopause Infographic
 libterm.com
libterm.com