Hypertrophic scars result from an overproduction of collagen during the healing process, leading to raised and thickened skin that remains within the boundaries of the original wound. These scars often cause discomfort, itching, and may restrict movement depending on their location. Discover effective treatments and prevention strategies in the rest of the article to help you manage hypertrophic scars successfully.
Table of Comparison
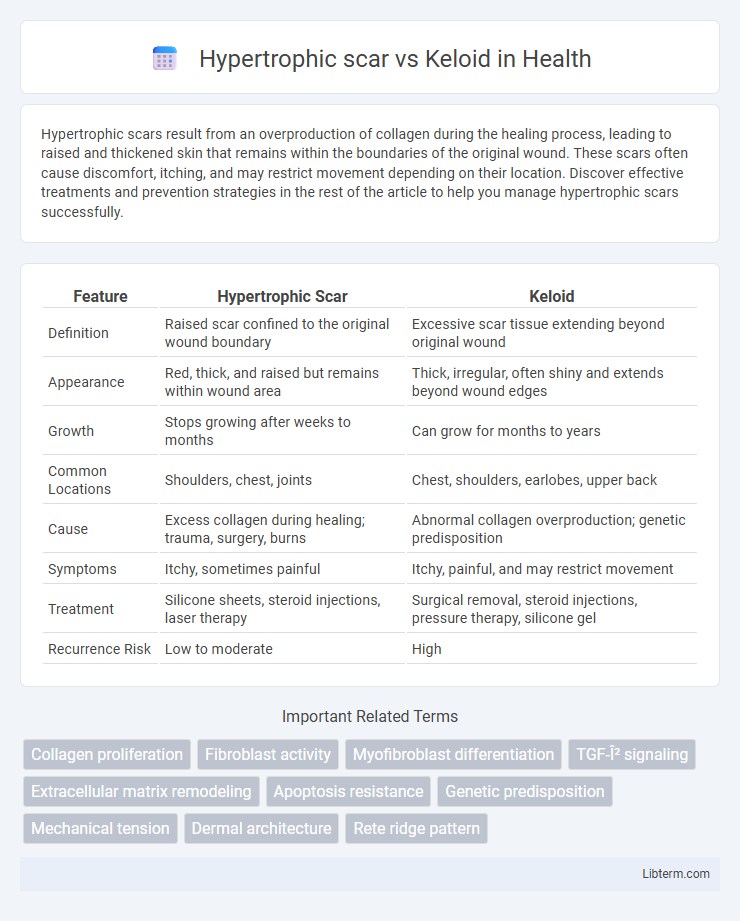
| Feature | Hypertrophic Scar | Keloid |
|---|---|---|
| Definition | Raised scar confined to the original wound boundary | Excessive scar tissue extending beyond original wound |
| Appearance | Red, thick, and raised but remains within wound area | Thick, irregular, often shiny and extends beyond wound edges |
| Growth | Stops growing after weeks to months | Can grow for months to years |
| Common Locations | Shoulders, chest, joints | Chest, shoulders, earlobes, upper back |
| Cause | Excess collagen during healing; trauma, surgery, burns | Abnormal collagen overproduction; genetic predisposition |
| Symptoms | Itchy, sometimes painful | Itchy, painful, and may restrict movement |
| Treatment | Silicone sheets, steroid injections, laser therapy | Surgical removal, steroid injections, pressure therapy, silicone gel |
| Recurrence Risk | Low to moderate | High |
Introduction to Hypertrophic Scars and Keloids
Hypertrophic scars and keloids are types of abnormal wound healing characterized by excessive collagen deposition. Hypertrophic scars remain confined to the boundaries of the original injury and often regress over time, while keloids extend beyond the wound margins and tend to persist indefinitely. Both conditions cause raised, fibrous tissue but differ in growth patterns and clinical management.
Key Differences Between Hypertrophic Scars and Keloids
Hypertrophic scars remain confined within the original wound boundaries, while keloids extend beyond these margins, growing aggressively into surrounding healthy skin. Hypertrophic scars typically develop within weeks after injury and often improve over time, whereas keloids may continue to enlarge for months or years and rarely regress without treatment. The cellular composition differs, with hypertrophic scars showing dense collagen aligned parallel to the skin surface, contrasting with the disorganized collagen bundles seen in keloids.
Causes and Risk Factors
Hypertrophic scars develop due to excessive collagen production confined within the original wound boundaries, commonly caused by trauma, surgery, or burns, with risk factors including fair skin, younger age, and wound infection. Keloids result from an overactive fibroblast response extending beyond the initial injury site, often triggered by skin injuries, piercings, or acne, with higher incidence in individuals with darker skin, family history, and certain genetic predispositions. Both conditions share inflammation and prolonged healing as critical contributors, but keloids show more aggressive growth and recurrence propensity.
Clinical Appearance and Diagnosis
Hypertrophic scars present as raised, red, and thickened tissue confined within the original wound boundaries, often regressing over time, while keloids extend beyond the wound margins with a more irregular shape and continue to grow. Clinically, hypertrophic scars are more common after burns and trauma and show less persistent inflammation compared to keloids, which are characterized by excessive collagen deposition and a genetic predisposition, especially in individuals with darker skin. Diagnosis relies on clinical examination supported by patient history, with biopsy reserved for atypical cases to differentiate between the two based on histopathological features such as fibroblast density and collagen arrangement.
Pathophysiology: How They Develop
Hypertrophic scars develop from excessive collagen production confined within the original wound boundaries due to prolonged inflammation and fibroblast activity. Keloids result from uncontrolled fibroblast proliferation and collagen deposition that extends beyond the initial injury site, driven by altered TGF-beta signaling and abnormal extracellular matrix remodeling. Both conditions involve dysregulated wound healing but differ in the extent of tissue growth and genetic predisposition.
Common Sites of Occurrence
Hypertrophic scars commonly develop on areas subjected to high tension such as the shoulders, chest, and back, often following surgical incisions or traumatic wounds. Keloids frequently occur on the earlobes, upper chest, shoulders, and cheeks, expanding beyond the original injury boundaries and more prevalent in individuals with darker skin tones. Both scar types can cause functional impairment and cosmetic concerns, but their distribution patterns help guide diagnosis and management.
Treatment Options for Hypertrophic Scars
Treatment options for hypertrophic scars include silicone gel sheets, corticosteroid injections, and laser therapy, which target collagen production and scar thickness. Pressure therapy and surgical revision may also be effective in reducing scar elevation and improving mobility. Emerging treatments like cryotherapy and laser-assisted drug delivery are gaining attention for enhancing scar remodeling and patient outcomes.
Treatment Options for Keloids
Keloid treatment options include intralesional corticosteroid injections, which reduce inflammation and fibroblast proliferation, making them the first-line therapy. Silicone gel sheets and pressure therapy aid in flattening and softening keloids by modulating collagen production. Surgical excision followed by adjuvant therapies like radiotherapy or cryotherapy minimizes recurrence rates in resistant or large keloids.
Prevention Strategies
Hypertrophic scar and keloid prevention strategies center on minimizing skin trauma and managing wound healing effectively. Applying silicone gel sheets, pressure therapy, and keeping wounds clean and moisturized can reduce excessive collagen formation linked to both hypertrophic scars and keloids. Early intervention with corticosteroid injections or laser therapy may also help prevent the progression of raised, fibrous scar tissue.
Prognosis and Long-term Management
Hypertrophic scars typically improve over time with conservative treatments such as pressure therapy, silicone gels, and corticosteroid injections, often becoming less noticeable within months to years. Keloids, in contrast, have a higher recurrence rate after treatment, requiring more aggressive and multimodal approaches including surgical excision combined with radiation or intralesional corticosteroids to manage symptoms and prevent regrowth. Long-term management of keloids often involves vigilant monitoring and repeated interventions, whereas hypertrophic scars generally stabilize with fewer interventions and a better overall prognosis.
Hypertrophic scar Infographic
 libterm.com
libterm.com