Onychomycosis and paronychia are common nail infections that can cause discoloration, thickening, and pain in the affected nails. Understanding the differences in symptoms, causes, and treatment options for these conditions is essential for effective management. Explore the rest of the article to learn how you can identify and treat these nail disorders properly.
Table of Comparison
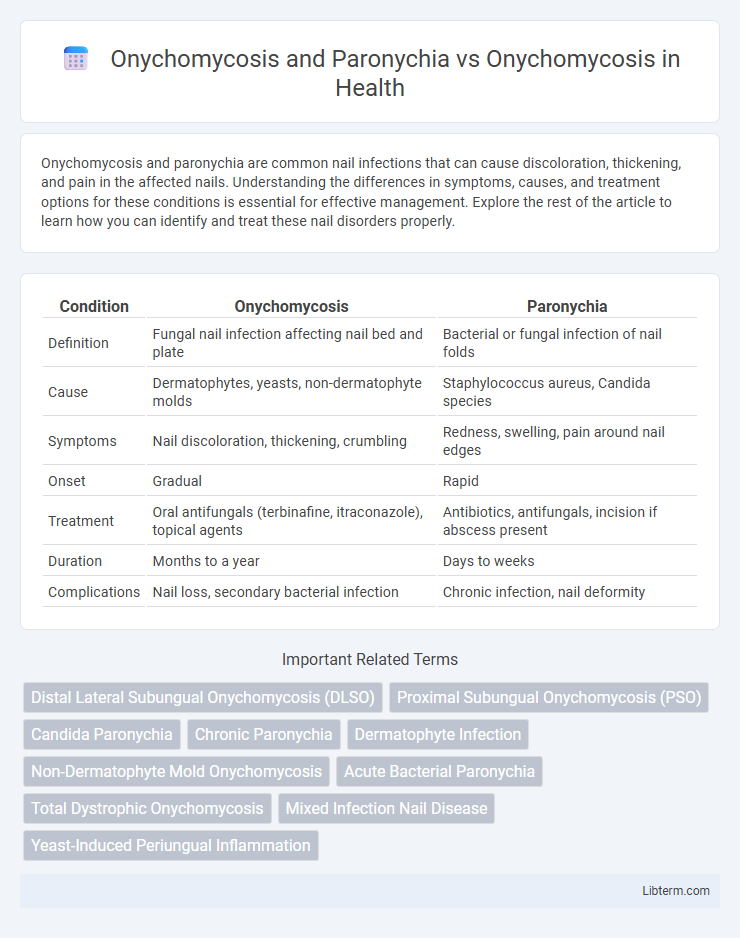
| Condition | Onychomycosis | Paronychia |
|---|---|---|
| Definition | Fungal nail infection affecting nail bed and plate | Bacterial or fungal infection of nail folds |
| Cause | Dermatophytes, yeasts, non-dermatophyte molds | Staphylococcus aureus, Candida species |
| Symptoms | Nail discoloration, thickening, crumbling | Redness, swelling, pain around nail edges |
| Onset | Gradual | Rapid |
| Treatment | Oral antifungals (terbinafine, itraconazole), topical agents | Antibiotics, antifungals, incision if abscess present |
| Duration | Months to a year | Days to weeks |
| Complications | Nail loss, secondary bacterial infection | Chronic infection, nail deformity |
Understanding Onychomycosis: Causes and Symptoms
Onychomycosis is a fungal infection affecting the nails, commonly caused by dermatophytes, yeasts, and non-dermatophyte molds, leading to nail discoloration, thickening, and brittleness. Paronychia is an infection of the nail folds caused primarily by bacteria or fungi, resulting in redness, swelling, and pain around the nail, differentiating it from the nail plate-centered Onychomycosis. Recognizing these symptoms is critical for accurate diagnosis and effective treatment, as Onychomycosis primarily impairs nail integrity while Paronychia presents with acute inflammatory signs.
What is Paronychia? Differentiating from Onychomycosis
Paronychia is an inflammation of the nail fold, often caused by bacterial or fungal infection, characterized by redness, swelling, and pain around the nail, unlike Onychomycosis which specifically involves fungal infection of the nail plate or nail bed leading to thickened, discolored, and brittle nails. Onychomycosis primarily affects nail aesthetics and integrity, while Paronychia presents with acute or chronic soft tissue inflammation adjacent to the nail. Differentiating Paronychia from Onychomycosis relies on clinical signs: Paronychia shows periungual swelling and tenderness, whereas Onychomycosis demonstrates nail dystrophy without significant surrounding tissue inflammation.
Comparative Overview: Onychomycosis vs Paronychia
Onychomycosis is a fungal infection primarily affecting the nail plate, characterized by discoloration, thickening, and brittleness, whereas paronychia is an infection of the nail fold involving bacterial or fungal pathogens, resulting in redness, swelling, and pain. Onychomycosis often presents chronically with gradual nail deformity, while paronychia typically manifests acutely with localized inflammation around the nail margin. Diagnosis for onychomycosis relies on mycological culture or PCR, whereas paronychia diagnosis is clinical, sometimes supported by bacterial culture if abscess formation occurs.
Key Risk Factors for Onychomycosis
Key risk factors for onychomycosis include frequently damp or sweaty feet, nail trauma, pre-existing skin conditions like psoriasis, and compromised immune systems such as in diabetes or HIV patients. Paronychia primarily results from bacterial or fungal infections due to nail fold injury or chronic exposure to moisture, distinguishing it from onychomycosis, which is a fungal infection of the nail plate. Understanding these risk factors is critical for preventing onychomycosis and differentiating it from paronychia in clinical diagnosis.
Common Triggers and Risk Factors for Paronychia
Paronychia commonly arises from bacterial or fungal infections due to nail trauma, frequent hand exposure to water, or manicuring injuries, contrasting with Onychomycosis primarily linked to dermatophyte fungi affecting the nail plate. Risk factors for Paronychia include chronic irritation, compromised immune response, and occupation-related handwork, while Onychomycosis risk increases with age, diabetes, and peripheral vascular disease. Both conditions share environmental elements such as humid climates but differ in their pathogenesis and primary infection sites.
Clinical Presentation: Nail Changes in Onychomycosis vs Paronychia
Onychomycosis manifests as thickened, discolored, brittle, and crumbly nails, often with subungual debris and nail plate separation. Paronychia is characterized by inflammation, redness, swelling, and tenderness around the nail folds, sometimes with pus formation, but usually without significant nail plate discoloration or thickening. Distinguishing nail changes in onychomycosis versus paronychia is crucial for accurate diagnosis and appropriate antifungal or antibacterial treatment.
Diagnosis: How to Identify Onychomycosis and Paronychia
Onychomycosis diagnosis involves direct microscopic examination of nail clippings stained with potassium hydroxide (KOH) and fungal cultures to confirm dermatophyte infection, while paronychia diagnosis relies on clinical evaluation of erythema, swelling around the nail folds, and sometimes bacterial cultures for acute cases. Differentiating onychomycosis from paronychia requires assessing nail plate changes such as discoloration, thickening, and nail bed debris typical of fungal infection versus the periungual inflammation characteristic of paronychia. Advanced diagnostic tools include PCR assays for fungal DNA in onychomycosis and ultrasound imaging to evaluate abscess formation in paronychia cases.
Treatment Options for Onychomycosis
Onychomycosis treatment primarily involves systemic antifungal medications such as terbinafine or itraconazole, which provide higher efficacy compared to topical treatments like ciclopirox or efinaconazole. In contrast, paronychia, often caused by bacterial infection, requires antibiotics or drainage rather than antifungals, highlighting the importance of accurate diagnosis. Laser therapy and nail debridement serve as adjunctive treatments for onychomycosis, especially in resistant cases or when systemic therapy is contraindicated.
Managing and Treating Paronychia
Managing and treating paronychia involves prompt identification and targeted therapy, often including warm soaks, topical or systemic antibiotics for bacterial infections, and antifungal agents when fungal involvement is suspected. In contrast to onychomycosis, which primarily requires prolonged antifungal treatment targeting dermatophytes, paronychia treatment focuses on reducing acute inflammation and addressing the causative pathogen, commonly Staphylococcus aureus or Candida species. Effective management of paronychia prevents chronic nail deformities and recurrence by combining proper hygiene, drainage of abscesses if present, and sometimes corticosteroid use to reduce inflammation.
Prevention Tips: Reducing the Risk of Nail Infections
Maintaining dry and clean nails is crucial in preventing onychomycosis and paronychia, as moisture creates an ideal environment for fungal and bacterial growth. Regularly trimming nails straight across and avoiding nail trauma minimizes the risk of infection by reducing entry points for pathogens. Wearing breathable footwear and gloves in wet or damp conditions further lowers the chances of developing these common nail infections.
Onychomycosis and Paronychia Infographic
 libterm.com
libterm.com