Pleural effusion occurs when excess fluid accumulates between the layers of the pleura surrounding the lungs, leading to symptoms like chest pain and difficulty breathing. Diagnosing this condition typically involves imaging tests such as chest X-rays or ultrasound, along with fluid analysis to determine the underlying cause. Discover how recognizing early signs and effective treatments can improve your health by reading the rest of the article.
Table of Comparison
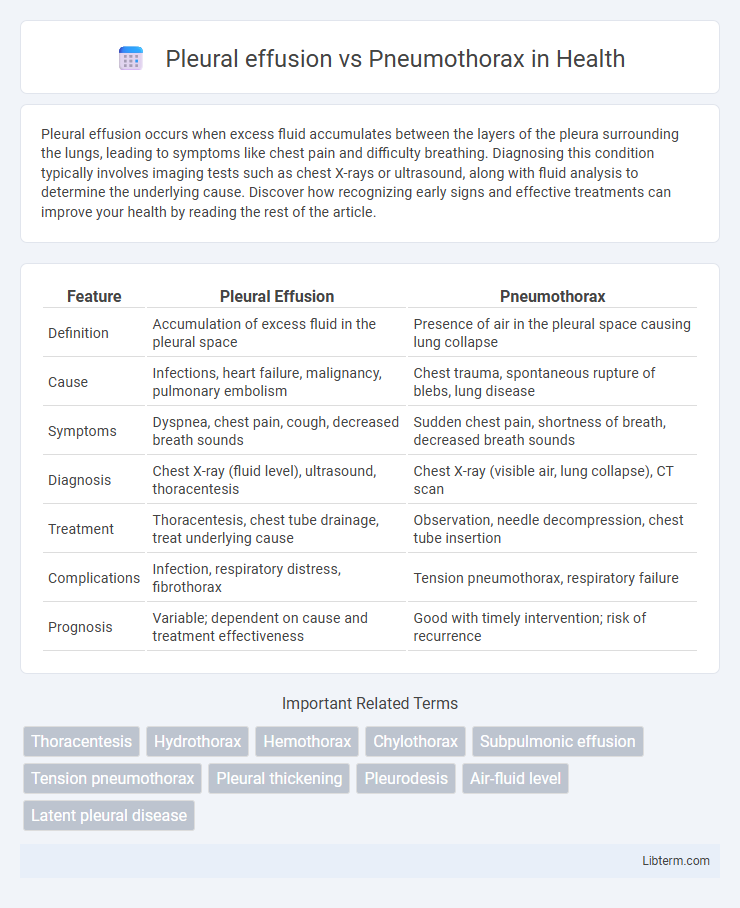
| Feature | Pleural Effusion | Pneumothorax |
|---|---|---|
| Definition | Accumulation of excess fluid in the pleural space | Presence of air in the pleural space causing lung collapse |
| Cause | Infections, heart failure, malignancy, pulmonary embolism | Chest trauma, spontaneous rupture of blebs, lung disease |
| Symptoms | Dyspnea, chest pain, cough, decreased breath sounds | Sudden chest pain, shortness of breath, decreased breath sounds |
| Diagnosis | Chest X-ray (fluid level), ultrasound, thoracentesis | Chest X-ray (visible air, lung collapse), CT scan |
| Treatment | Thoracentesis, chest tube drainage, treat underlying cause | Observation, needle decompression, chest tube insertion |
| Complications | Infection, respiratory distress, fibrothorax | Tension pneumothorax, respiratory failure |
| Prognosis | Variable; dependent on cause and treatment effectiveness | Good with timely intervention; risk of recurrence |
Overview of Pleural Effusion and Pneumothorax
Pleural effusion is the accumulation of excess fluid between the layers of the pleura surrounding the lungs, often caused by conditions such as congestive heart failure, pneumonia, or malignancy. Pneumothorax involves the presence of air in the pleural space, leading to lung collapse, typically resulting from trauma, spontaneous rupture of lung blebs, or underlying lung disease. Both conditions disrupt normal lung function but differ in their etiology, presentation on imaging, and management approaches.
Definitions and Key Differences
Pleural effusion is the accumulation of excess fluid in the pleural cavity surrounding the lungs, whereas pneumothorax involves the presence of air in the pleural space, leading to lung collapse. The key difference is that pleural effusion causes lung compression due to fluid buildup, while pneumothorax results from air-induced pressure disrupting lung expansion. Diagnostic imaging such as chest X-rays and ultrasounds clearly distinguish pleural effusion's fluid layering from pneumothorax's visible air gap and lung edge separation.
Causes and Risk Factors
Pleural effusion commonly arises from congestive heart failure, pneumonia, malignancies, and pulmonary embolism, with risk factors including chronic lung diseases and infections. Pneumothorax is primarily caused by trauma, underlying lung disorders like chronic obstructive pulmonary disease (COPD), and spontaneous ruptures of subpleural blebs, with risk factors such as smoking, tall stature, and previous pneumothorax episodes. Both conditions involve the pleural space but differ significantly in etiology, influencing clinical management and outcomes.
Clinical Presentations
Pleural effusion typically presents with dyspnea, decreased breath sounds, and dullness to percussion on the affected side, often accompanied by pleuritic chest pain. Pneumothorax manifests with sudden onset unilateral chest pain, absent breath sounds, hyperresonance on percussion, and respiratory distress in severe cases. Both conditions impair lung expansion but require distinct clinical assessment and intervention strategies.
Diagnostic Imaging and Tests
Pleural effusion is typically diagnosed through chest X-rays, revealing fluid accumulation in the pleural space, with ultrasound providing precise localization and volume estimation, while CT scans offer detailed images of underlying causes. Pneumothorax is commonly identified by chest X-rays showing the presence of air in the pleural cavity with lung collapse, and CT scans are used for detecting small or occult pneumothorax and assessing severity. Ultrasound can rapidly detect both conditions at the bedside, particularly useful in emergency settings for guiding immediate interventions.
Pathophysiological Mechanisms
Pleural effusion involves the accumulation of excess fluid in the pleural space due to imbalances in hydrostatic and oncotic pressures, lymphatic obstruction, or increased capillary permeability, leading to impaired lung expansion and gas exchange. Pneumothorax results from air entering the pleural cavity, often caused by trauma or spontaneous alveolar rupture, which disrupts the negative pressure necessary to keep the lung inflated, causing lung collapse. Both conditions alter the pleural pressure dynamics but differ fundamentally in the nature of the intrapleural content--fluid in pleural effusion versus air in pneumothorax--resulting in distinct respiratory pathophysiology.
Treatment and Management Strategies
Treatment of pleural effusion typically involves thoracentesis for fluid drainage and addressing the underlying cause, such as infection or malignancy, with antibiotics or chemotherapy. Pneumothorax management depends on severity; small, stable pneumothoraxes may resolve with observation and oxygen therapy, while larger or tension pneumothoraxes require urgent needle decompression or chest tube insertion. Both conditions necessitate prompt diagnosis with chest X-rays or ultrasound and ongoing monitoring to prevent complications like respiratory distress or recurrent effusions.
Complications and Prognosis
Pleural effusion complications include respiratory distress, infection leading to empyema, and fibrothorax causing pleural thickening, which may result in chronic lung impairment. Pneumothorax complications involve tension pneumothorax, causing life-threatening cardiovascular compromise, and recurrent episodes that can lead to persistent air leaks and lung collapse. Prognosis for pleural effusion depends on underlying cause and treatment timeliness, while pneumothorax prognosis varies by size and intervention, with tension pneumothorax requiring urgent management to prevent mortality.
Prevention and Patient Education
Prevention of pleural effusion involves managing underlying causes such as heart failure, infections, and malignancies through timely medical treatment and lifestyle modifications like smoking cessation and fluid management. Educating patients on recognizing early symptoms including chest pain, shortness of breath, and persistent cough facilitates prompt medical evaluation to prevent complications. For pneumothorax, prevention centers on avoiding risk factors such as smoking, trauma, and certain medical procedures, while patient education emphasizes the importance of seeking immediate care when experiencing sudden chest pain or respiratory distress to reduce recurrence and severity.
Frequently Asked Questions (FAQs)
Pleural effusion is the accumulation of excess fluid in the pleural space, whereas pneumothorax involves the presence of air in the pleural cavity, leading to lung collapse. Common FAQs address causes, with pleural effusion often resulting from heart failure, infections, or malignancy, and pneumothorax frequently caused by trauma, lung disease, or spontaneous rupture. Diagnostic differences include pleural effusion showing fluid on chest X-ray and ultrasound, while pneumothorax presents as a visible air pocket and absence of lung markings on imaging.
Pleural effusion Infographic
 libterm.com
libterm.com