Hypoxemia occurs when the level of oxygen in your blood is abnormally low, leading to symptoms such as shortness of breath, rapid heartbeat, and confusion. It can result from various conditions affecting the lungs, heart, or blood circulation, requiring timely diagnosis and treatment to prevent serious complications. Explore the rest of this article to understand the causes, symptoms, and effective management of hypoxemia.
Table of Comparison
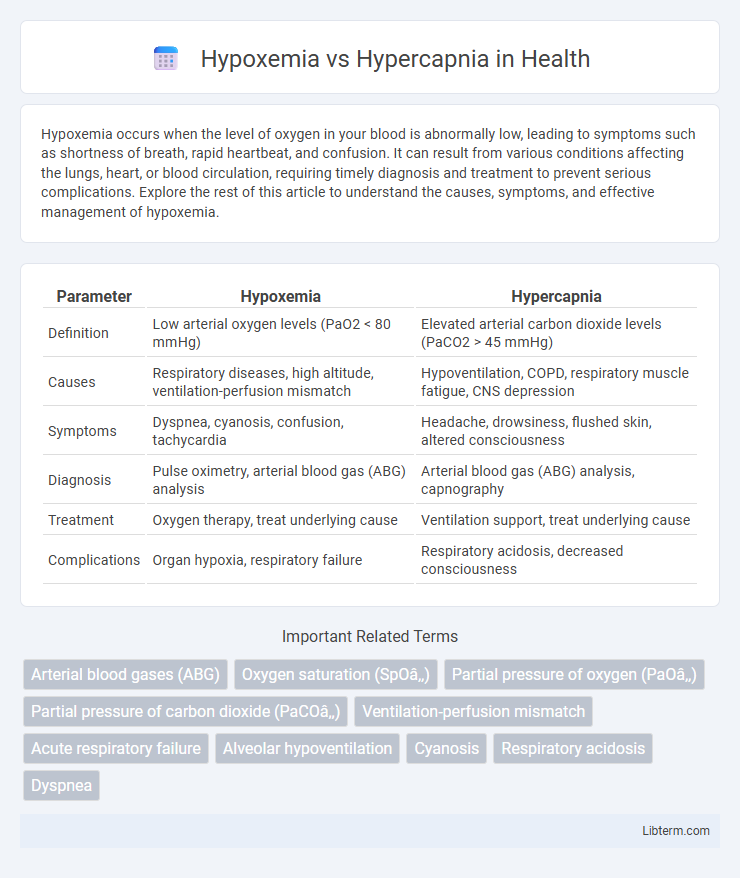
| Parameter | Hypoxemia | Hypercapnia |
|---|---|---|
| Definition | Low arterial oxygen levels (PaO2 < 80 mmHg) | Elevated arterial carbon dioxide levels (PaCO2 > 45 mmHg) |
| Causes | Respiratory diseases, high altitude, ventilation-perfusion mismatch | Hypoventilation, COPD, respiratory muscle fatigue, CNS depression |
| Symptoms | Dyspnea, cyanosis, confusion, tachycardia | Headache, drowsiness, flushed skin, altered consciousness |
| Diagnosis | Pulse oximetry, arterial blood gas (ABG) analysis | Arterial blood gas (ABG) analysis, capnography |
| Treatment | Oxygen therapy, treat underlying cause | Ventilation support, treat underlying cause |
| Complications | Organ hypoxia, respiratory failure | Respiratory acidosis, decreased consciousness |
Understanding Hypoxemia: Definition and Causes
Hypoxemia is characterized by abnormally low levels of oxygen in the arterial blood, typically defined by a partial pressure of oxygen (PaO2) below 80 mm Hg. Common causes include respiratory disorders such as chronic obstructive pulmonary disease (COPD), pneumonia, pulmonary embolism, and conditions that impair oxygen diffusion like interstitial lung disease. Understanding hypoxemia is essential for differentiating it from hypercapnia, where elevated carbon dioxide levels (PaCO2 > 45 mm Hg) indicate hypoventilation or impaired CO2 elimination.
What is Hypercapnia? Key Concepts Explained
Hypercapnia is a medical condition characterized by elevated levels of carbon dioxide (CO2) in the bloodstream, often resulting from inadequate respiration or impaired gas exchange in the lungs. It can cause symptoms such as shortness of breath, headaches, dizziness, and confusion, and is commonly associated with chronic obstructive pulmonary disease (COPD), hypoventilation, or respiratory failure. Understanding hypercapnia involves recognizing its impact on acid-base balance, as excessive CO2 increases blood acidity, leading to respiratory acidosis that requires prompt medical intervention.
Pathophysiology: Hypoxemia vs Hypercapnia
Hypoxemia occurs due to impaired oxygen exchange or decreased oxygen availability, leading to low arterial oxygen tension (PaO2) primarily caused by ventilation-perfusion mismatch, diffusion defects, or hypoventilation. Hypercapnia results from inadequate removal of carbon dioxide (PaCO2 elevation) often due to hypoventilation, reduced respiratory drive, or increased dead space ventilation. Both conditions disrupt cellular metabolism, with hypoxemia impairing aerobic respiration and hypercapnia causing respiratory acidosis and potential central nervous system depression.
Clinical Manifestations: Comparing Symptoms
Hypoxemia presents with symptoms such as cyanosis, tachycardia, confusion, and shortness of breath, reflecting insufficient oxygen in the blood. Hypercapnia typically causes headache, flushed skin, dyspnea, and altered mental status due to elevated carbon dioxide levels. Both conditions may lead to respiratory distress, but cyanosis is more prominent in hypoxemia, while hypercapnia often results in increased respiratory rate and somnolence.
Common Causes of Hypoxemia and Hypercapnia
Hypoxemia commonly arises from conditions like chronic obstructive pulmonary disease (COPD), pneumonia, pulmonary embolism, and high-altitude exposure, all of which impair oxygen exchange in the lungs. Hypercapnia typically results from hypoventilation due to respiratory depression, severe asthma, chronic bronchitis, or neuromuscular disorders that reduce the ability to expel carbon dioxide effectively. Both conditions reflect underlying respiratory dysfunction but differ in their primary disturbances--oxygen deficiency in hypoxemia versus carbon dioxide retention in hypercapnia.
Diagnostic Approaches: Differentiating the Conditions
Diagnostic approaches for hypoxemia and hypercapnia primarily involve arterial blood gas (ABG) analysis, which measures oxygen (PaO2) and carbon dioxide (PaCO2) levels to distinguish between low blood oxygen and elevated carbon dioxide levels. Pulse oximetry serves as a non-invasive initial assessment tool for hypoxemia by estimating oxygen saturation, whereas capnography provides continuous monitoring of CO2 levels to detect hypercapnia, especially in ventilated patients. Imaging studies and pulmonary function tests complement these diagnostics by identifying underlying respiratory conditions contributing to either hypoxemia or hypercapnia.
Acute vs Chronic Presentations
Hypoxemia, characterized by low arterial oxygen levels, presents acutely with symptoms such as cyanosis, tachypnea, and confusion, while chronic hypoxemia often leads to polycythemia, clubbing, and pulmonary hypertension. Hypercapnia, defined by elevated arterial carbon dioxide, manifests acutely through headaches, drowsiness, and respiratory acidosis, whereas chronic hypercapnia typically results in compensatory metabolic alkalosis and symptoms like morning headaches and fatigue. Differentiating acute versus chronic presentations involves assessing blood gas values, clinical signs, and compensatory mechanisms to guide appropriate management strategies.
Complications and Health Impacts
Hypoxemia, characterized by low blood oxygen levels, can lead to tissue hypoxia, organ dysfunction, and increased risk of cardiovascular events such as arrhythmias and myocardial infarction. Hypercapnia, defined by elevated carbon dioxide in the blood, often results in respiratory acidosis, altered mental status, and can cause severe complications including respiratory failure and increased intracranial pressure. Both conditions significantly impact respiratory and neurological health, requiring prompt diagnosis and targeted management to prevent long-term morbidity and mortality.
Management Strategies and Treatment Options
Management strategies for hypoxemia prioritize oxygen therapy to increase arterial oxygen saturation, often employing nasal cannulas, face masks, or mechanical ventilation in severe cases. Hypercapnia treatment focuses on enhancing alveolar ventilation through non-invasive ventilation methods like BiPAP or invasive mechanical ventilation to remove excess CO2. Both conditions require addressing underlying causes such as respiratory infections, COPD exacerbations, or neuromuscular disorders to optimize gas exchange and improve patient outcomes.
Prevention and Risk Reduction Measures
Preventing hypoxemia and hypercapnia involves maintaining optimal oxygenation and ventilation through lifestyle modifications, such as avoiding smoking and managing chronic respiratory conditions like COPD and asthma. Regular monitoring with pulse oximetry and arterial blood gas analysis aids early detection, allowing timely interventions like supplemental oxygen therapy and ventilatory support. Risk reduction also entails vaccination against respiratory infections and ensuring adherence to prescribed treatments to improve lung function and reduce complications.
Hypoxemia Infographic
 libterm.com
libterm.com