Oligoarthritis is a form of arthritis characterized by inflammation affecting two to four joints, often leading to pain, swelling, and stiffness. It commonly impacts the knees, ankles, and wrists, and can vary in severity depending on the underlying cause. Discover more about the symptoms, diagnosis, and treatment options for managing your condition in the rest of this article.
Table of Comparison
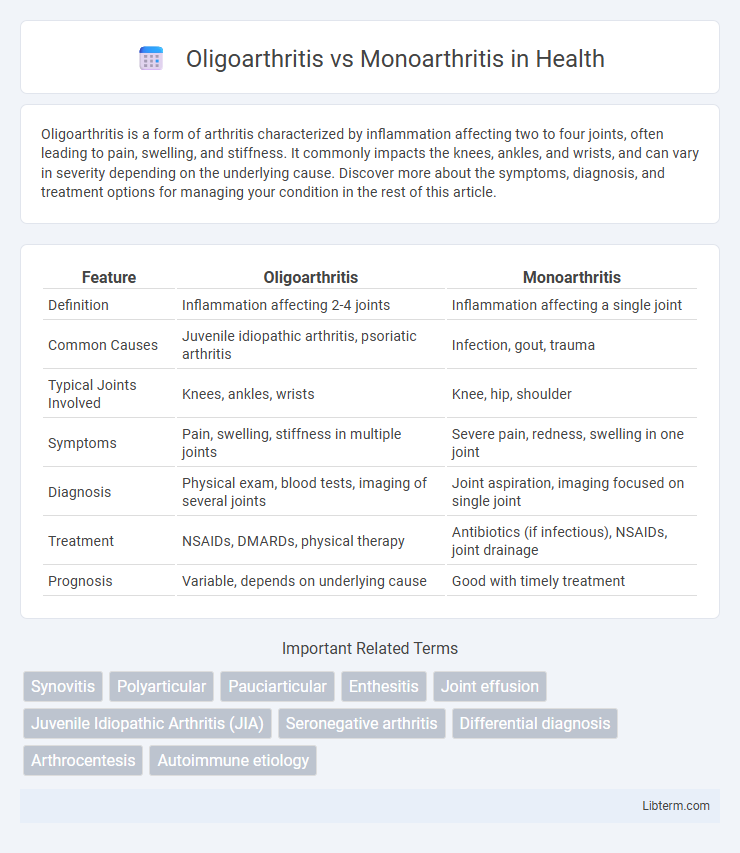
| Feature | Oligoarthritis | Monoarthritis |
|---|---|---|
| Definition | Inflammation affecting 2-4 joints | Inflammation affecting a single joint |
| Common Causes | Juvenile idiopathic arthritis, psoriatic arthritis | Infection, gout, trauma |
| Typical Joints Involved | Knees, ankles, wrists | Knee, hip, shoulder |
| Symptoms | Pain, swelling, stiffness in multiple joints | Severe pain, redness, swelling in one joint |
| Diagnosis | Physical exam, blood tests, imaging of several joints | Joint aspiration, imaging focused on single joint |
| Treatment | NSAIDs, DMARDs, physical therapy | Antibiotics (if infectious), NSAIDs, joint drainage |
| Prognosis | Variable, depends on underlying cause | Good with timely treatment |
Understanding Oligoarthritis and Monoarthritis
Oligoarthritis is characterized by inflammation affecting two to four joints, commonly seen in juvenile idiopathic arthritis and often involving larger joints like knees and ankles. Monoarthritis involves inflammation in a single joint, frequently caused by trauma, infection, or crystalline arthropathies such as gout. Differentiating these conditions relies on clinical evaluation, joint aspiration, and imaging studies to identify the underlying etiology and guide targeted treatment.
Key Differences Between Oligoarthritis and Monoarthritis
Oligoarthritis involves inflammation in two to four joints within the first six months of disease onset, commonly affecting larger joints like knees and ankles, while monoarthritis is characterized by inflammation confined to a single joint. Oligoarthritis is frequently seen in juvenile idiopathic arthritis and may present with mild systemic symptoms, whereas monoarthritis often suggests infectious, crystal-induced, or early degenerative causes. Diagnosis and treatment strategies differ, with oligoarthritis requiring screening for uveitis and potential systemic therapy, while monoarthritis often mandates urgent joint aspiration and targeted antimicrobial or anti-inflammatory management.
Common Causes of Oligoarthritis
Oligoarthritis typically involves inflammation in two to four joints and is commonly caused by juvenile idiopathic arthritis, psoriatic arthritis, or reactive arthritis, often triggered by infections or autoimmune reactions. Unlike monoarthritis, which affects a single joint and is frequently caused by gout, trauma, or septic arthritis, oligoarthritis usually presents with symmetric joint involvement and may indicate systemic inflammatory conditions. Accurate diagnosis requires clinical evaluation supported by laboratory tests such as ESR, CRP, and joint fluid analysis to differentiate these distinct arthritis types and their underlying causes.
Common Causes of Monoarthritis
Monoarthritis typically results from infections such as septic arthritis caused by Staphylococcus aureus or from crystal-induced inflammation like gout and pseudogout, which deposit monosodium urate or calcium pyrophosphate crystals in the joint. Traumatic injury and early stages of inflammatory arthritis, including rheumatoid arthritis and psoriatic arthritis, may also present as monoarthritis. In contrast, oligoarthritis involves inflammation of two to four joints and is often linked to juvenile idiopathic arthritis, spondyloarthropathies, or reactive arthritis following infections.
Typical Symptoms and Clinical Presentation
Oligoarthritis commonly presents with inflammation in 2 to 4 joints, often involving larger joints such as the knees and ankles, accompanied by symptoms like joint swelling, stiffness, and limited range of motion. Monoarthritis typically affects a single joint, most frequently the knee, and presents with acute pain, swelling, redness, and warmth, which may indicate infection or crystal arthropathy. Both conditions can cause joint stiffness, but the number of affected joints and underlying causes help differentiate the diagnosis.
Diagnosis: Oligoarthritis vs Monoarthritis
Diagnosis of oligoarthritis involves identifying inflammation in two to four joints, often confirmed through clinical evaluation, blood tests for markers like ESR and CRP, and imaging studies such as ultrasound or MRI to detect synovitis. In contrast, monoarthritis diagnosis focuses on a single affected joint, with synovial fluid analysis playing a crucial role to differentiate between infectious, crystal-induced, or inflammatory causes. Accurate differentiation between oligoarthritis and monoarthritis guides targeted treatment strategies and helps identify underlying conditions like juvenile idiopathic arthritis or septic arthritis.
Treatment Approaches for Oligoarthritis
Treatment approaches for oligoarthritis primarily involve the use of nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce inflammation and pain, alongside intra-articular corticosteroid injections to target affected joints directly. Disease-modifying antirheumatic drugs (DMARDs), such as methotrexate, are prescribed when oligoarthritis persists or extends beyond a few joints, aiming to prevent joint damage and control systemic symptoms. Physical therapy is integrated to maintain joint function and mobility, distinguishing oligoarthritis management from the typically more localized treatment of monoarthritis.
Treatment Approaches for Monoarthritis
Treatment approaches for monoarthritis primarily target the underlying cause, such as infection, crystal-induced inflammation, or autoimmune disorders. Nonsteroidal anti-inflammatory drugs (NSAIDs) effectively reduce pain and inflammation, while corticosteroid injections provide localized relief. In infectious cases, appropriate antibiotic therapy is critical, whereas joint aspiration and rest are important supportive measures to prevent joint damage and improve function.
Prognosis and Long-Term Outcomes
Oligoarthritis typically involves four or fewer joints within the first six months and often has a better long-term prognosis, especially in juvenile idiopathic arthritis, where many patients experience remission or minimal joint damage. Monoarthritis affects a single joint and can have variable outcomes depending on the underlying cause, such as infection, trauma, or inflammatory diseases; untreated monoarthritis can lead to joint destruction and chronic disability. Early diagnosis and appropriate treatment are crucial in both conditions to improve long-term function and prevent irreversible joint damage.
When to Seek Medical Attention
Seek medical attention for oligoarthritis or monoarthritis if joint pain, swelling, and stiffness persist beyond a few days or worsen, especially if accompanied by fever, redness, or severe limitation in movement. Early diagnosis is crucial to prevent joint damage in conditions like juvenile idiopathic arthritis or septic arthritis. Immediate evaluation is necessary if symptoms involve multiple joints or if there is sudden onset of severe pain or systemic symptoms indicating infection or autoimmune disease.
Oligoarthritis Infographic
 libterm.com
libterm.com