Carcinoma and melanoma are two primary types of skin cancer, with carcinoma originating from epithelial cells and melanoma developing from pigment-producing melanocytes. Early detection and treatment are crucial for improving survival rates and minimizing complications. Explore the rest of the article to understand the differences, risk factors, and effective prevention strategies for these skin cancers.
Table of Comparison
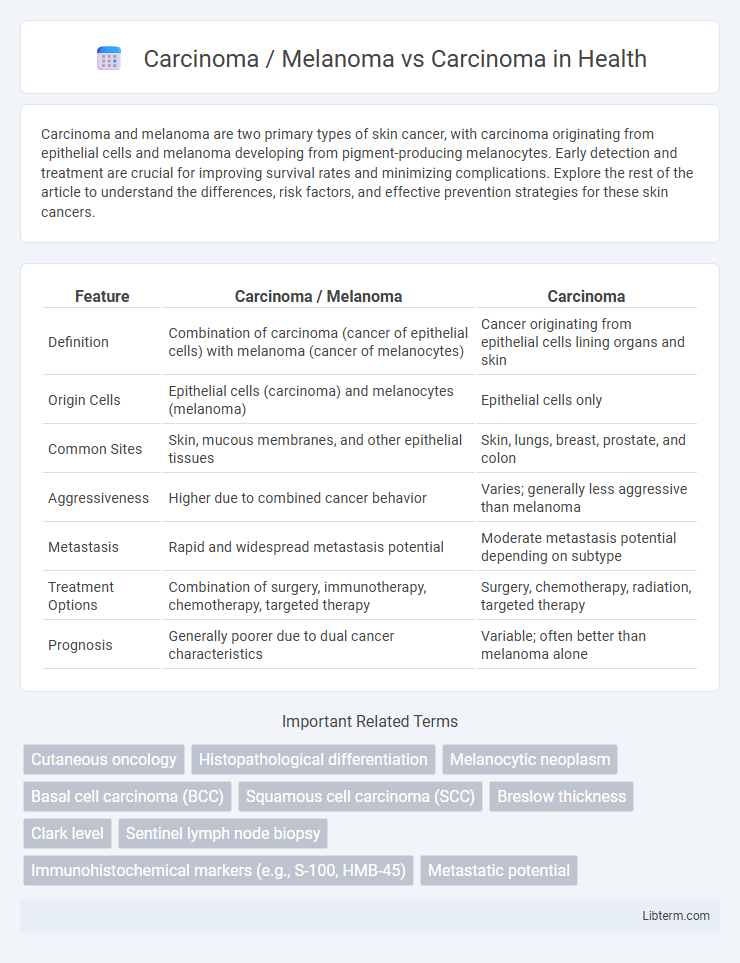
| Feature | Carcinoma / Melanoma | Carcinoma |
|---|---|---|
| Definition | Combination of carcinoma (cancer of epithelial cells) with melanoma (cancer of melanocytes) | Cancer originating from epithelial cells lining organs and skin |
| Origin Cells | Epithelial cells (carcinoma) and melanocytes (melanoma) | Epithelial cells only |
| Common Sites | Skin, mucous membranes, and other epithelial tissues | Skin, lungs, breast, prostate, and colon |
| Aggressiveness | Higher due to combined cancer behavior | Varies; generally less aggressive than melanoma |
| Metastasis | Rapid and widespread metastasis potential | Moderate metastasis potential depending on subtype |
| Treatment Options | Combination of surgery, immunotherapy, chemotherapy, targeted therapy | Surgery, chemotherapy, radiation, targeted therapy |
| Prognosis | Generally poorer due to dual cancer characteristics | Variable; often better than melanoma alone |
Introduction to Carcinoma and Melanoma
Carcinoma is a type of cancer originating from epithelial cells, responsible for forming the lining of organs and tissues, and accounts for nearly 80-90% of all cancer cases. Melanoma, a subtype of carcinoma, arises specifically from melanocytes, the pigment-producing cells in the skin, and is much less common but highly aggressive. Understanding the cellular origin and behavior of carcinoma and melanoma is essential for accurate diagnosis and targeted treatment strategies.
Defining Carcinoma: Types and Origins
Carcinoma is a malignant tumor arising from epithelial cells that line organs and tissues, with major types including squamous cell carcinoma, adenocarcinoma, and basal cell carcinoma. Melanoma, a distinct form of cancer, originates specifically from melanocytes, the pigment-producing cells in the skin, and differs significantly in behavior and treatment from carcinomas. Understanding the origins of carcinoma is critical for accurate diagnosis and targeted therapy, as its types vary based on the epithelial tissue involved and anatomical location.
Understanding Melanoma: Key Characteristics
Melanoma is a malignant tumor originating from melanocytes, characterized by rapid growth and a high potential for metastasis compared to typical carcinomas, which arise from epithelial cells. Key characteristics of melanoma include asymmetrical shape, irregular borders, multiple colors, and a diameter larger than 6 millimeters, often identified using the ABCDE criteria (Asymmetry, Border, Color, Diameter, Evolving). Early detection and precise diagnosis through biopsy and dermatoscopy are critical for improving prognosis and treatment outcomes.
Carcinoma vs Melanoma: Cellular Differences
Carcinoma originates from epithelial cells, characterized by abnormal proliferation and invasion of tissues lining organs and glands, while melanoma arises from melanocytes, the pigment-producing cells in the skin. Cellular differences include carcinoma cells often forming glandular or squamous patterns, whereas melanoma cells display high melanin production and irregular dendritic shapes. Melanoma cells exhibit greater genetic mutations and aggressive metastatic potential compared to the typically more localized carcinoma cells.
Risk Factors for Carcinoma and Melanoma
Carcinoma risk factors primarily include prolonged exposure to ultraviolet (UV) radiation, smoking, chronic inflammation, and genetic predispositions such as mutations in tumor suppressor genes like TP53. Melanoma risk factors are heavily linked to intense intermittent UV exposure, presence of multiple or atypical nevi, fair skin with a tendency to sunburn, and familial history involving CDKN2A gene mutations. Both carcinomas and melanomas share UV radiation as a common environmental risk, but melanoma's aggressive nature corresponds with specific genetic and phenotypic markers distinct from other carcinoma types.
Clinical Presentation and Symptoms
Carcinoma typically presents as a persistent lump, non-healing ulcer, or unexplained weight loss, often affecting epithelial tissues such as the lungs, breasts, or colon. Melanoma, a malignant tumor of melanocytes, frequently manifests as a changing mole with asymmetry, irregular borders, color variation, diameter over 6mm, and evolving characteristics (ABCDE criteria). Early clinical symptoms of melanoma include localized itching, bleeding, or tenderness, distinguishing it from carcinoma which may remain asymptomatic until advanced stages.
Diagnostic Methods: Carcinoma vs Melanoma
Diagnostic methods for carcinoma typically include biopsy with histopathological examination, imaging techniques like CT, MRI, and PET scans to assess tumor size and metastasis, and tumor marker analysis for specific carcinoma types such as PSA for prostate cancer. Melanoma diagnosis relies heavily on dermoscopy for detailed skin lesion inspection, followed by excisional biopsy to evaluate the depth and stage through Breslow thickness and Clark level, with sentinel lymph node biopsy often performed to detect regional metastasis. Molecular testing and immunohistochemistry play critical roles in differentiating melanoma from carcinoma and guiding targeted therapies.
Treatment Options for Both Cancers
Treatment options for carcinoma primarily include surgery, radiation therapy, chemotherapy, and targeted therapies based on tumor location and stage. Melanoma treatment strategies often involve surgical excision, immunotherapy agents like checkpoint inhibitors (e.g., pembrolizumab, nivolumab), targeted therapies for BRAF-mutated tumors, and adjuvant radiation in advanced cases. Emerging therapies and clinical trials focus on personalized treatment approaches, improving survival rates for both carcinoma and melanoma.
Prognosis and Survival Rates Comparison
Melanoma generally has a better prognosis and higher survival rates compared to many carcinomas, especially when detected early, with a 5-year survival rate exceeding 90% for localized melanoma. In contrast, carcinomas such as pancreatic or lung cancer often show lower survival rates, frequently below 20% at five years due to late-stage diagnosis and aggressive behavior. Early detection and treatment significantly improve outcomes for both melanoma and carcinomas, but melanoma's responsiveness to immunotherapy and targeted therapies further enhances its survival odds.
Prevention and Early Detection Strategies
Prevention and early detection strategies for melanoma and carcinoma differ due to their distinct origins and risk factors; melanoma prevention emphasizes rigorous sun protection, including the use of broad-spectrum sunscreen, protective clothing, and avoiding tanning beds, while carcinoma prevention often targets risk factors such as smoking cessation and reducing exposure to carcinogens. Early detection of melanoma relies heavily on regular skin self-examinations using the ABCDE criteria (Asymmetry, Border irregularity, Color variation, Diameter, and Evolution) and periodic dermatological screenings, whereas carcinoma detection typically depends on tissue biopsies following abnormal findings in clinical examinations or imaging studies. Effective public health campaigns and advancements in diagnostic technologies enhance early intervention, improving prognosis and survival rates for both melanoma and carcinoma patients.
Carcinoma / Melanoma Infographic
 libterm.com
libterm.com