Hypocalcemia is a condition characterized by abnormally low levels of calcium in the blood, which can lead to muscle cramps, spasms, and cardiac issues. Proper diagnosis and treatment are essential to manage symptoms and prevent complications related to bone health and nerve function. Explore the rest of the article to understand hypocalcemia's causes, symptoms, and effective treatment options tailored for your well-being.
Table of Comparison
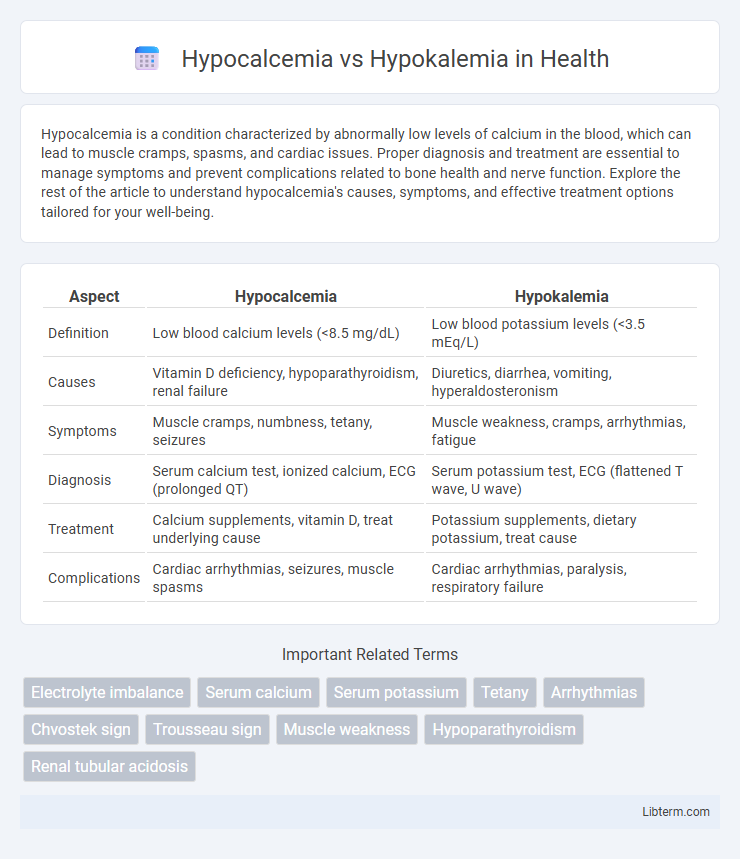
| Aspect | Hypocalcemia | Hypokalemia |
|---|---|---|
| Definition | Low blood calcium levels (<8.5 mg/dL) | Low blood potassium levels (<3.5 mEq/L) |
| Causes | Vitamin D deficiency, hypoparathyroidism, renal failure | Diuretics, diarrhea, vomiting, hyperaldosteronism |
| Symptoms | Muscle cramps, numbness, tetany, seizures | Muscle weakness, cramps, arrhythmias, fatigue |
| Diagnosis | Serum calcium test, ionized calcium, ECG (prolonged QT) | Serum potassium test, ECG (flattened T wave, U wave) |
| Treatment | Calcium supplements, vitamin D, treat underlying cause | Potassium supplements, dietary potassium, treat cause |
| Complications | Cardiac arrhythmias, seizures, muscle spasms | Cardiac arrhythmias, paralysis, respiratory failure |
Introduction to Hypocalcemia and Hypokalemia
Hypocalcemia is a condition characterized by abnormally low levels of calcium in the blood, typically below 8.5 mg/dL, leading to symptoms such as muscle cramps, tetany, and cardiac arrhythmias. Hypokalemia refers to potassium deficiency in the bloodstream, with serum potassium levels falling below 3.5 mEq/L, resulting in muscle weakness, fatigue, and potential cardiac disturbances. Both electrolyte imbalances disrupt cellular function and require prompt diagnosis and treatment to prevent serious complications.
Defining Hypocalcemia: Causes and Risk Factors
Hypocalcemia is defined by low calcium levels in the blood, typically below 8.5 mg/dL, often resulting from vitamin D deficiency, hypoparathyroidism, or chronic kidney disease. Risk factors include malabsorption syndromes, certain medications like bisphosphonates, and post-surgical complications affecting the parathyroid glands. Understanding the causes and risk factors helps differentiate hypocalcemia from hypokalemia, which involves low potassium levels rather than calcium abnormalities.
Defining Hypokalemia: Causes and Risk Factors
Hypokalemia, defined as a serum potassium level below 3.5 mmol/L, results from potassium loss due to factors such as diuretic use, gastrointestinal losses, or inadequate dietary intake. Risk factors include chronic kidney disease, excessive sweating, and certain endocrine disorders like hyperaldosteronism. Understanding these causes is essential for distinguishing hypokalemia from hypocalcemia, which involves low calcium levels and different clinical implications.
Common Symptoms of Hypocalcemia
Hypocalcemia typically presents with symptoms such as muscle cramps, tetany, and numbness or tingling in the fingers and around the mouth. These manifestations result from low serum calcium levels affecting neuromuscular excitability. Unlike hypokalemia, which primarily causes muscle weakness, hypocalcemia's hallmark symptoms involve increased neuromuscular irritability and positive Chvostek's and Trousseau's signs.
Common Symptoms of Hypokalemia
Hypokalemia commonly presents with muscle weakness, cramps, fatigue, and arrhythmias due to low potassium levels disrupting cellular function. In contrast, hypocalcemia primarily causes symptoms like muscle spasms, tetany, and numbness owing to calcium deficiency affecting nerve excitability. Recognizing hypokalemia's hallmark clinical features, such as muscle paralysis and ECG changes including flattened T waves and U waves, is critical for accurate diagnosis and treatment.
Key Differences Between Hypocalcemia and Hypokalemia
Hypocalcemia is characterized by low calcium levels in the blood, leading to symptoms like muscle cramps, numbness, and tetany, while hypokalemia involves low potassium levels, causing muscle weakness, cramps, and cardiac arrhythmias. The underlying causes differ significantly; hypocalcemia often results from vitamin D deficiency, hypoparathyroidism, or chronic kidney disease, whereas hypokalemia is commonly due to diuretic use, gastrointestinal losses, or excessive aldosterone. Laboratory tests reveal distinct electrolyte imbalances with serum calcium below 8.5 mg/dL in hypocalcemia and serum potassium under 3.5 mEq/L in hypokalemia, necessitating targeted treatment based on the specific electrolyte disturbance.
Diagnostic Approaches for Hypocalcemia and Hypokalemia
Diagnostic approaches for hypocalcemia include measuring serum total and ionized calcium levels, alongside assessments of parathyroid hormone (PTH), vitamin D, and phosphate concentrations to identify underlying causes such as hypoparathyroidism or vitamin D deficiency. In hypokalemia, diagnosis involves serum potassium measurement complemented by evaluating renal potassium excretion through urine potassium tests and acid-base status to distinguish between renal and extrarenal potassium losses. Both conditions require ECG monitoring to detect characteristic cardiac changes, aiding in the assessment of severity and guiding urgent management.
Treatment Options: Hypocalcemia vs Hypokalemia
Treatment options for hypocalcemia primarily include calcium supplementation either orally or intravenously, along with vitamin D analogs to enhance calcium absorption. Hypokalemia management focuses on potassium replacement through oral or intravenous potassium chloride while addressing underlying causes like diuretics or gastrointestinal losses. Monitoring electrolyte levels and the patient's cardiac function is essential in both conditions to prevent complications such as arrhythmias.
Complications and Long-Term Effects
Hypocalcemia can lead to complications such as muscle spasms, tetany, and cardiac arrhythmias, with long-term effects including osteoporosis and impaired neurological function. Hypokalemia increases the risk of muscle weakness, cardiac arrhythmias, and paralysis, potentially causing chronic kidney damage and metabolic alkalosis over time. Both electrolyte imbalances require prompt detection to prevent severe cardiovascular and neuromuscular complications.
Prevention Strategies and Patient Education
Prevention of hypocalcemia centers on maintaining adequate dietary calcium and vitamin D intake while monitoring patients at risk, such as those with chronic kidney disease or post-thyroidectomy, to avoid complications. Hypokalemia prevention involves ensuring sufficient potassium intake through diet or supplementation, especially in patients on diuretics or with conditions causing excessive potassium loss. Educating patients on recognizing symptoms like muscle cramps for hypocalcemia and weakness or arrhythmias for hypokalemia supports early intervention and adherence to treatment protocols.
Hypocalcemia Infographic
 libterm.com
libterm.com