Frailty is a common clinical syndrome characterized by decreased strength, endurance, and physiological function, increasing vulnerability to adverse health outcomes in older adults. Addressing frailty involves interventions such as physical exercise, nutrition optimization, and careful management of chronic conditions. Discover how understanding frailty can improve your health and wellbeing by exploring the rest of this article.
Table of Comparison
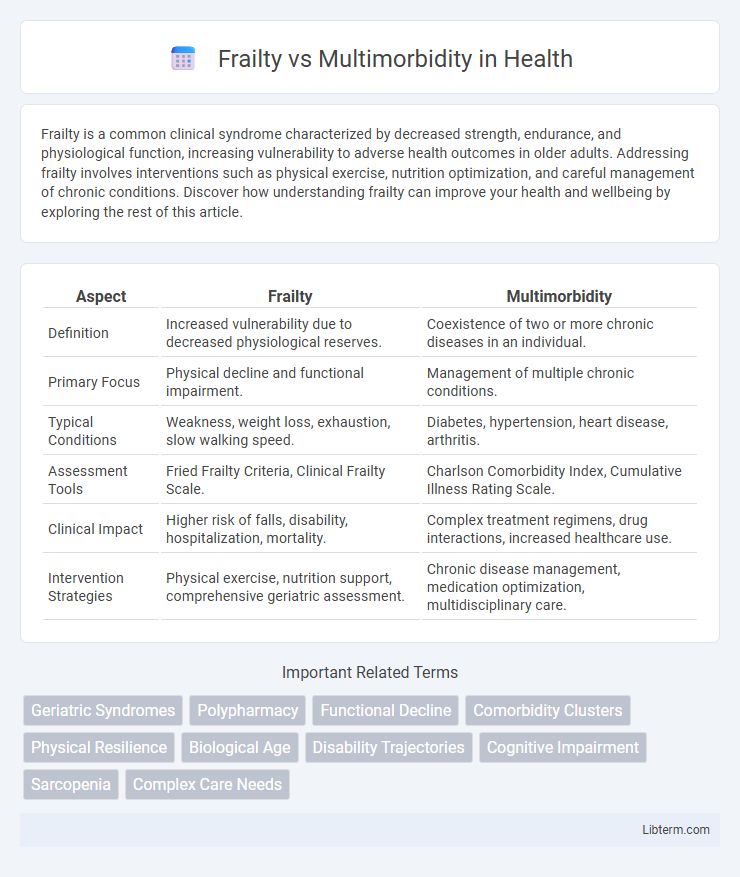
| Aspect | Frailty | Multimorbidity |
|---|---|---|
| Definition | Increased vulnerability due to decreased physiological reserves. | Coexistence of two or more chronic diseases in an individual. |
| Primary Focus | Physical decline and functional impairment. | Management of multiple chronic conditions. |
| Typical Conditions | Weakness, weight loss, exhaustion, slow walking speed. | Diabetes, hypertension, heart disease, arthritis. |
| Assessment Tools | Fried Frailty Criteria, Clinical Frailty Scale. | Charlson Comorbidity Index, Cumulative Illness Rating Scale. |
| Clinical Impact | Higher risk of falls, disability, hospitalization, mortality. | Complex treatment regimens, drug interactions, increased healthcare use. |
| Intervention Strategies | Physical exercise, nutrition support, comprehensive geriatric assessment. | Chronic disease management, medication optimization, multidisciplinary care. |
Understanding Frailty: Definition and Key Characteristics
Frailty is a clinical syndrome characterized by diminished strength, endurance, and reduced physiological function, increasing an individual's vulnerability to adverse health outcomes. Core features include unintentional weight loss, weakness, exhaustion, slow walking speed, and low physical activity. Unlike multimorbidity, which involves the presence of multiple chronic diseases, frailty specifically reflects a state of decreased resilience and biological aging.
Multimorbidity: What It Means and Why It Matters
Multimorbidity refers to the coexistence of two or more chronic conditions in an individual, significantly impacting health outcomes and healthcare management. It poses challenges such as increased complexity in treatment, higher risk of adverse drug interactions, and greater healthcare utilization. Understanding multimorbidity is crucial for developing personalized care plans and improving quality of life in aging populations.
Differences Between Frailty and Multimorbidity
Frailty is characterized by decreased physiological reserve and increased vulnerability to stressors, resulting in a higher risk of adverse health outcomes, whereas multimorbidity refers to the coexistence of two or more chronic diseases in an individual. Frailty primarily reflects diminished physical and functional capacity, often measured by criteria like unintentional weight loss, weakness, and slow walking speed, while multimorbidity involves the cumulative burden of chronic conditions such as diabetes, hypertension, and arthritis. Understanding the distinctions aids in tailored clinical management, as frailty impacts prognosis and intervention strategies differently from multimorbidity.
Overlapping Features: Where Frailty and Multimorbidity Meet
Frailty and multimorbidity share overlapping features such as increased vulnerability to adverse health outcomes, reduced physiological reserve, and higher risk of hospitalization and mortality in older adults. Both conditions involve multiple organ systems and contribute to functional decline, impaired mobility, and cognitive impairment. Understanding their intersection enhances clinical assessment and individualized care planning to improve health outcomes in aging populations.
Assessment Tools for Frailty and Multimorbidity
Assessment tools for frailty often include the Frailty Phenotype, which evaluates criteria such as unintentional weight loss, exhaustion, and low physical activity, and the Frailty Index that quantifies deficits across multiple health domains. Multimorbidity assessment typically employs tools like the Charlson Comorbidity Index and Cumulative Illness Rating Scale, which measure the number and severity of coexisting chronic diseases. Combining frailty and multimorbidity assessments provides a comprehensive understanding of patient vulnerability and guides personalized clinical interventions.
Clinical Implications: Diagnosis and Management
Frailty and multimorbidity significantly impact clinical decision-making, requiring distinct diagnostic criteria and tailored management strategies to optimize patient outcomes. Frailty is characterized by decreased physiological reserves, assessed through tools like the Frailty Phenotype or Frailty Index, necessitating interventions aimed at improving functional status and preventing adverse events such as falls and hospitalizations. Multimorbidity involves the coexistence of multiple chronic diseases, often managed through comprehensive care plans emphasizing medication optimization, coordinated specialty input, and addressing patient-centered goals to reduce treatment burden and enhance quality of life.
Impact on Patient Outcomes: Frailty vs Multimorbidity
Frailty significantly increases the risk of adverse outcomes such as falls, hospitalization, and mortality by compromising physiological reserves, while multimorbidity complicates disease management and polypharmacy, elevating the risk of drug interactions and healthcare utilization. Studies show frail patients have higher rates of functional decline and dependency compared to those with multimorbidity alone. Effective interventions targeting frailty can improve patient outcomes more substantially than disease-specific treatments in multimorbid populations.
Preventive Strategies for Older Adults
Preventive strategies for frailty in older adults emphasize resistance training, balanced nutrition rich in protein and vitamins, and routine health screenings to identify early functional decline. Multimorbidity prevention involves comprehensive management of chronic conditions such as diabetes, hypertension, and cardiovascular diseases through medication adherence, lifestyle modifications, and regular monitoring to reduce disease progression. Integrated care models combining physical activity, dietary interventions, and coordinated medical oversight effectively address both frailty and multimorbidity, improving quality of life and reducing hospitalization rates in the elderly population.
Future Research Directions in Aging Care
Future research in aging care must prioritize distinguishing the complex interactions between frailty and multimorbidity to develop targeted interventions. Longitudinal studies utilizing biomarkers and comprehensive geriatric assessments can elucidate progression pathways and identify modifiable risk factors. Integrating personalized medicine approaches and advanced data analytics will enhance predictive models for better clinical decision-making and resource allocation in elderly populations.
Conclusion: Integrating Care for Frailty and Multimorbidity
Integrating care for frailty and multimorbidity enhances patient outcomes by addressing complex health needs through multidisciplinary approaches, personalized care plans, and comprehensive assessments. Coordinated interventions target both physical vulnerability and multiple chronic conditions, reducing hospitalizations and improving quality of life. Emphasizing collaboration among healthcare providers enables proactive management, preventing decline and supporting functional independence in elderly populations.
Frailty Infographic
 libterm.com
libterm.com