Neutropenia is a condition characterized by an abnormally low number of neutrophils, a type of white blood cell essential for fighting infections. It can lead to increased susceptibility to bacterial and fungal infections, making early diagnosis and management critical. Explore the rest of this article to learn about causes, symptoms, and treatment options to protect your health.
Table of Comparison
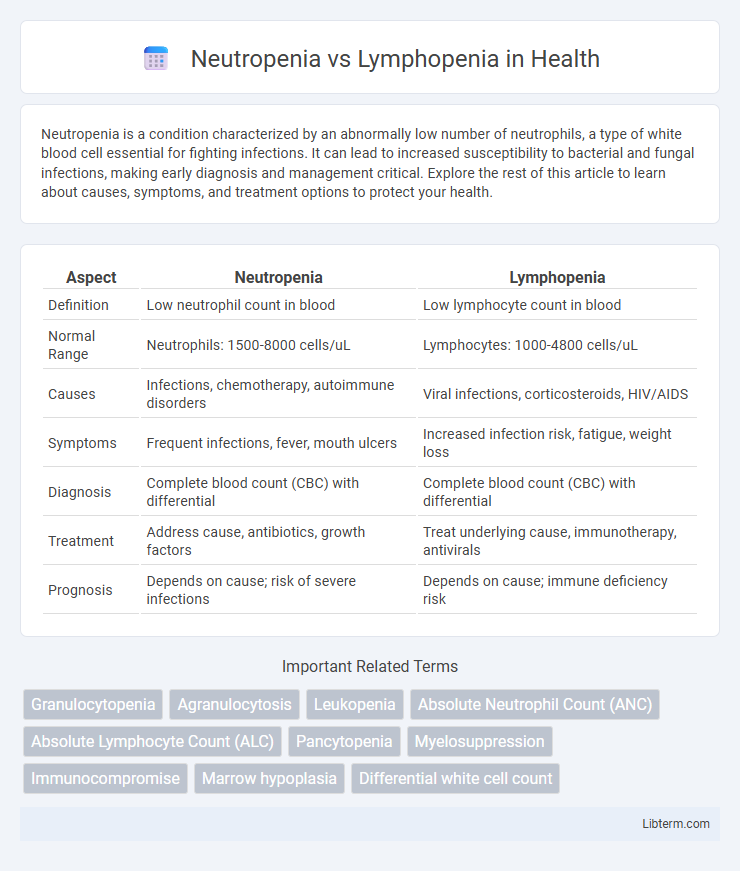
| Aspect | Neutropenia | Lymphopenia |
|---|---|---|
| Definition | Low neutrophil count in blood | Low lymphocyte count in blood |
| Normal Range | Neutrophils: 1500-8000 cells/uL | Lymphocytes: 1000-4800 cells/uL |
| Causes | Infections, chemotherapy, autoimmune disorders | Viral infections, corticosteroids, HIV/AIDS |
| Symptoms | Frequent infections, fever, mouth ulcers | Increased infection risk, fatigue, weight loss |
| Diagnosis | Complete blood count (CBC) with differential | Complete blood count (CBC) with differential |
| Treatment | Address cause, antibiotics, growth factors | Treat underlying cause, immunotherapy, antivirals |
| Prognosis | Depends on cause; risk of severe infections | Depends on cause; immune deficiency risk |
Introduction to Neutropenia and Lymphopenia
Neutropenia is characterized by an abnormally low count of neutrophils, a type of white blood cell crucial for combating bacterial infections. Lymphopenia involves a decreased number of lymphocytes, which play a vital role in immune response against viral infections and in adaptive immunity. Both conditions indicate compromised immune function but affect different cellular components with distinct clinical implications.
Definitions: What Is Neutropenia?
Neutropenia is a hematological condition characterized by an abnormally low count of neutrophils, a type of white blood cell essential for combating bacterial infections. This deficit can result from various causes, including bone marrow disorders, chemotherapy, or autoimmune diseases, increasing the risk of severe infections. Neutrophil counts below 1,500 cells per microliter typically define neutropenia, distinguishing it from other leukocyte abnormalities such as lymphopenia.
Definitions: What Is Lymphopenia?
Lymphopenia, also known as lymphocytopenia, is a condition characterized by an abnormally low level of lymphocytes in the blood, which are critical white blood cells involved in the immune response. Neutropenia, in contrast, refers to a deficiency in neutrophils, another type of white blood cell essential for combating bacterial infections. Both conditions indicate compromised immune function but affect different components of the white blood cell population, with lymphopenia impacting adaptive immunity and neutropenia primarily impairing innate immune defense.
Key Differences Between Neutropenia and Lymphopenia
Neutropenia is characterized by an abnormally low count of neutrophils, which are crucial for fighting bacterial infections, whereas lymphopenia involves a reduced number of lymphocytes, key players in adaptive immunity against viruses and tumors. Neutropenia often results from chemotherapy, bone marrow disorders, or severe infections, leading to increased susceptibility to bacterial and fungal infections; lymphopenia is commonly associated with viral infections, autoimmune diseases, or immunodeficiency conditions like HIV/AIDS. Diagnostic differentiation relies on complete blood count (CBC) with differential, revealing specific declines in neutrophils for neutropenia and lymphocytes for lymphopenia, guiding tailored treatment approaches.
Causes of Neutropenia
Neutropenia primarily results from bone marrow disorders, autoimmune diseases, severe infections like sepsis, chemotherapy, or certain medications that suppress neutrophil production. In contrast, lymphopenia often arises due to viral infections, immunodeficiency disorders such as HIV/AIDS, or corticosteroid therapy. Understanding the distinct causes helps guide appropriate diagnostic evaluations and targeted treatments for each condition.
Causes of Lymphopenia
Lymphopenia primarily results from viral infections such as HIV, which directly target lymphocytes, or from autoimmune disorders like lupus that cause lymphocyte destruction. Other causes include malnutrition, corticosteroid treatment, and congenital immunodeficiency disorders that impair lymphocyte production or function. Distinguishing lymphopenia from neutropenia involves analyzing different etiologies since neutropenia is often related to bacterial infections, chemotherapy, or bone marrow suppression.
Clinical Manifestations and Symptoms
Neutropenia often presents with frequent bacterial infections, fever, sore throat, and mouth ulcers due to decreased neutrophil count impairing the body's ability to fight bacterial pathogens. Lymphopenia is characterized by increased susceptibility to viral, fungal, and opportunistic infections, manifesting as recurrent respiratory infections, chronic diarrhea, and sometimes skin lesions. Both conditions can lead to severe infections but differ in the type of immune cells affected and corresponding clinical symptoms.
Diagnostic Approaches
Neutropenia diagnosis primarily involves a complete blood count (CBC) with differential to measure absolute neutrophil count (ANC), often complemented by bone marrow biopsy if severe or unexplained. Lymphopenia diagnosis also relies on CBC with differential to determine absolute lymphocyte count, with further testing including flow cytometry to identify specific lymphocyte subsets and underlying causes such as infections or immunodeficiencies. Both conditions may require additional serological and molecular assays to detect infections, autoimmune diseases, or hematologic malignancies influencing white blood cell abnormalities.
Treatment Strategies for Each Condition
Neutropenia treatment primarily involves addressing the underlying cause, such as infections or chemotherapy effects, with granulocyte colony-stimulating factor (G-CSF) to stimulate neutrophil production and prophylactic antibiotics to prevent infections. Lymphopenia management centers on treating the root issues like viral infections, autoimmune diseases, or immunodeficiency disorders, with therapies including immunoglobulin replacement or antiviral medications depending on the etiology. Both conditions require regular monitoring of blood cell counts and patient immune status to tailor treatment intensity and prevent complications effectively.
Prognosis and Long-Term Outcomes
Neutropenia often leads to a higher risk of bacterial infections, impacting prognosis with potential recurrent infections and the necessity for ongoing monitoring or prophylactic treatments. Lymphopenia is associated with impaired immune response, increasing susceptibility to viral infections and sometimes correlating with chronic conditions or malignancies, influencing long-term outcomes. Prognostic differences depend on the underlying cause, severity, and duration of each condition, with neutropenia typically posing more acute infectious risks while lymphopenia may indicate broader immune dysfunction.
Neutropenia Infographic
 libterm.com
libterm.com