Lymphadenopathy refers to the swelling or enlargement of lymph nodes, often signaling an underlying infection, inflammation, or malignancy. Identifying the cause involves a thorough medical history, physical examination, and sometimes imaging or biopsy. Discover how to recognize, diagnose, and manage lymphadenopathy to protect your health by reading the rest of this article.
Table of Comparison
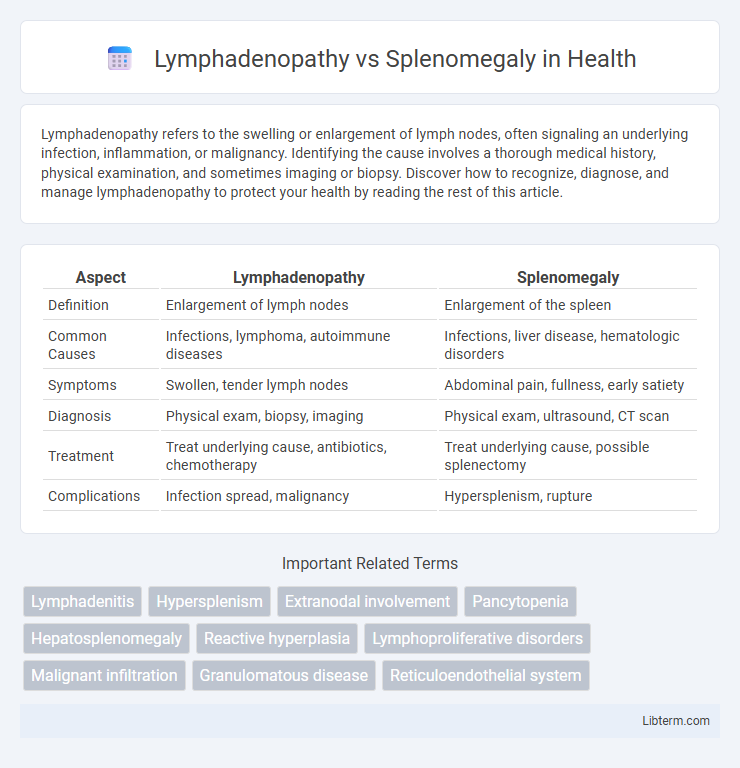
| Aspect | Lymphadenopathy | Splenomegaly |
|---|---|---|
| Definition | Enlargement of lymph nodes | Enlargement of the spleen |
| Common Causes | Infections, lymphoma, autoimmune diseases | Infections, liver disease, hematologic disorders |
| Symptoms | Swollen, tender lymph nodes | Abdominal pain, fullness, early satiety |
| Diagnosis | Physical exam, biopsy, imaging | Physical exam, ultrasound, CT scan |
| Treatment | Treat underlying cause, antibiotics, chemotherapy | Treat underlying cause, possible splenectomy |
| Complications | Infection spread, malignancy | Hypersplenism, rupture |
Introduction: Understanding Lymphadenopathy and Splenomegaly
Lymphadenopathy refers to the abnormal enlargement of lymph nodes caused by infections, autoimmune diseases, or malignancies, serving as a key indicator of immune response or pathology. Splenomegaly denotes an enlarged spleen resulting from conditions like liver disease, hematologic disorders, or infections, often reflecting systemic illness or hematopoietic abnormalities. Differentiating these conditions involves evaluating clinical presentation, imaging studies, and laboratory tests to guide diagnosis and treatment effectively.
Definitions and Core Concepts
Lymphadenopathy refers to the abnormal enlargement of lymph nodes, often due to infections, autoimmune diseases, or malignancies, and is characterized by palpable swelling in regions like the neck, armpits, or groin. Splenomegaly denotes an enlarged spleen, which results from conditions such as liver disease, hematologic disorders, or infections, leading to increased spleen size detectable via imaging or physical examination. Both conditions indicate underlying systemic issues affecting the lymphatic and reticuloendothelial systems but differ primarily in anatomical location and associated pathophysiology.
Causes of Lymphadenopathy
Lymphadenopathy primarily results from infections such as viral (e.g., Epstein-Barr virus, HIV), bacterial (e.g., tuberculosis, streptococcal infections), and fungal causes, as well as malignancies including lymphoma and metastatic cancer. Autoimmune diseases like systemic lupus erythematosus and rheumatoid arthritis also contribute to lymph node enlargement. Differentiating from splenomegaly, which often arises from hematologic disorders, liver diseases, and systemic infections, lymphadenopathy is localized to lymph nodes and reflects localized or systemic immune responses.
Causes of Splenomegaly
Splenomegaly, the enlargement of the spleen, is commonly caused by infections such as mononucleosis, bacterial endocarditis, and malaria, as well as hematologic diseases like leukemia, lymphoma, and hemolytic anemia. Other causes include liver diseases such as cirrhosis leading to portal hypertension, autoimmune disorders like systemic lupus erythematosus, and storage diseases including Gaucher's and Niemann-Pick disease. In contrast, lymphadenopathy primarily involves swollen lymph nodes due to infections, malignancies, or immune responses without direct spleen involvement.
Clinical Presentations and Symptoms
Lymphadenopathy presents primarily as enlarged, palpable lymph nodes often accompanied by localized pain or tenderness, fever, and symptoms of underlying infections or malignancies. Splenomegaly manifests as an enlarged spleen detectable on physical examination, causing abdominal fullness, left upper quadrant pain, early satiety, and symptoms related to hypersplenism such as anemia or thrombocytopenia. Both conditions may indicate systemic diseases, but their clinical presentations differ according to the affected lymphatic or hematopoietic tissues.
Diagnostic Approaches and Imaging
Diagnostic approaches for lymphadenopathy primarily include ultrasound for superficial lymph nodes and fine-needle aspiration biopsy to evaluate lymph node architecture and malignancy. Splenomegaly diagnosis relies on physical examination complemented by abdominal ultrasound, CT scan, or MRI to assess splenic size, texture, and involvement in systemic diseases. Advanced imaging such as PET-CT helps differentiate reactive lymphadenopathy from lymphoma and evaluates splenic lesions or infiltration.
Laboratory Findings and Differentiating Features
Lymphadenopathy typically presents with enlarged lymph nodes detectable via physical examination and ultrasound, often accompanied by elevated white blood cell counts or specific markers like lactate dehydrogenase (LDH) in cases of lymphoma. Splenomegaly is characterized by an enlarged spleen identifiable through palpation and confirmed by imaging modalities such as ultrasound or CT scan, frequently associated with hematologic abnormalities including anemia, thrombocytopenia, or elevated liver enzymes depending on the underlying cause. Differentiating features include the anatomical location of enlargement--localized nodes in lymphadenopathy versus diffuse splenic enlargement--and distinct laboratory profiles, where lymphadenopathy shows localized immune response markers, while splenomegaly often reflects systemic hematopoietic or infiltrative disorders.
Common Diseases Associated with Each Condition
Lymphadenopathy commonly occurs in infections such as mononucleosis, tuberculosis, and bacterial lymphadenitis, as well as malignancies like lymphoma and leukemia. Splenomegaly is frequently associated with hematologic diseases including myeloproliferative disorders, hemolytic anemia, and infections like malaria or viral hepatitis. Both conditions signal underlying systemic pathology but affect different components of the lymphoreticular system.
Treatment and Management Strategies
Lymphadenopathy treatment varies based on underlying causes, ranging from antibiotics for infections to chemotherapy or immunotherapy for malignancies. Splenomegaly management depends on etiology, including addressing infections, blood disorders, or autoimmune diseases, with splenectomy reserved for severe or refractory cases. Regular monitoring and supportive care are essential in both conditions to manage symptoms and prevent complications.
Prognosis and Complications
Lymphadenopathy prognosis varies depending on the underlying cause, such as infection, malignancy, or autoimmune disease, with complications including chronic inflammation or lymphoma progression. Splenomegaly often signals systemic conditions like hematologic disorders or infections and may lead to complications such as hypersplenism, causing pancytopenia or increased risk of splenic rupture. Early diagnosis and targeted management are critical to improve outcomes and prevent severe sequelae in both lymphadenopathy and splenomegaly.
Lymphadenopathy Infographic
 libterm.com
libterm.com