Pheochromocytoma is a rare tumor that develops in the adrenal glands, causing excessive production of adrenaline and noradrenaline. Symptoms often include high blood pressure, headaches, sweating, and rapid heartbeat, which can lead to serious cardiovascular complications if untreated. Discover more about diagnosis, treatment options, and how you can manage this condition by reading the full article.
Table of Comparison
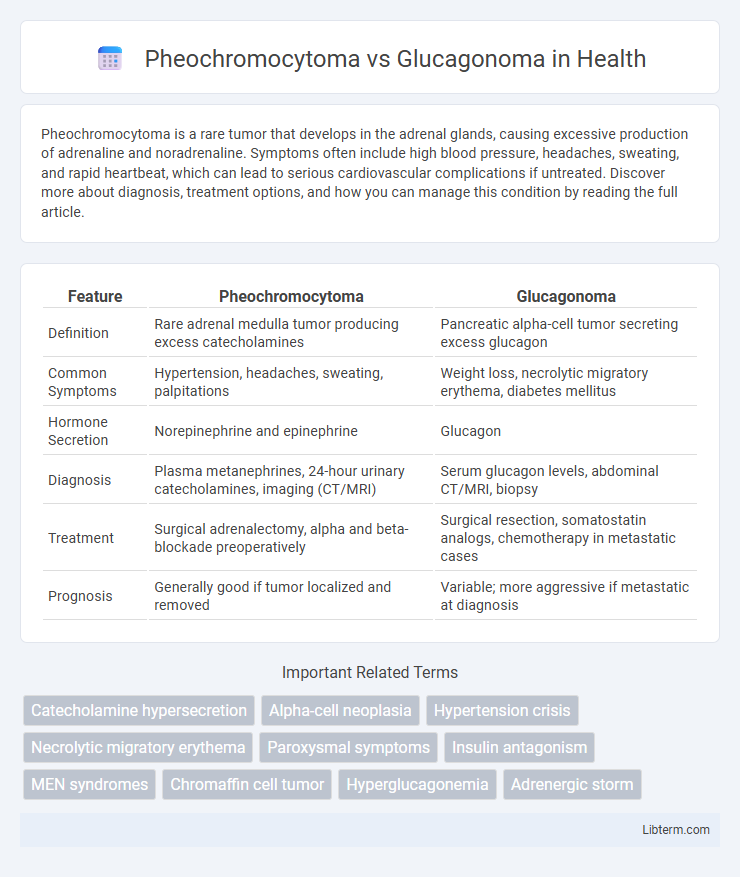
| Feature | Pheochromocytoma | Glucagonoma |
|---|---|---|
| Definition | Rare adrenal medulla tumor producing excess catecholamines | Pancreatic alpha-cell tumor secreting excess glucagon |
| Common Symptoms | Hypertension, headaches, sweating, palpitations | Weight loss, necrolytic migratory erythema, diabetes mellitus |
| Hormone Secretion | Norepinephrine and epinephrine | Glucagon |
| Diagnosis | Plasma metanephrines, 24-hour urinary catecholamines, imaging (CT/MRI) | Serum glucagon levels, abdominal CT/MRI, biopsy |
| Treatment | Surgical adrenalectomy, alpha and beta-blockade preoperatively | Surgical resection, somatostatin analogs, chemotherapy in metastatic cases |
| Prognosis | Generally good if tumor localized and removed | Variable; more aggressive if metastatic at diagnosis |
Overview of Pheochromocytoma and Glucagonoma
Pheochromocytoma is a rare catecholamine-secreting tumor originating from adrenal medulla chromaffin cells, causing symptoms like hypertension, palpitations, and headaches due to excess adrenaline and noradrenaline. In contrast, Glucagonoma is an uncommon neuroendocrine tumor of pancreatic alpha cells, characterized by overproduction of glucagon leading to hyperglycemia, weight loss, and necrolytic migratory erythema. Both tumors require biochemical testing and imaging for diagnosis but differ significantly in clinical presentation and metabolic effects.
Causes and Risk Factors
Pheochromocytoma is primarily caused by tumors originating in the adrenal medulla, often linked to genetic mutations in RET, VHL, or NF1 genes, with risk factors including hereditary syndromes like Multiple Endocrine Neoplasia type 2 (MEN 2). In contrast, Glucagonoma arises from alpha cells of the pancreatic islets, frequently associated with somatic mutations in the MEN1 gene. Both tumors exhibit hormonal hypersecretion leading to distinct clinical syndromes, with genetic predisposition playing a critical role in their pathogenesis.
Pathophysiology: Key Differences
Pheochromocytoma arises from chromaffin cells in the adrenal medulla, leading to excessive secretion of catecholamines such as norepinephrine and epinephrine, causing hypertension and episodic symptoms like palpitations, sweating, and headaches. Glucagonoma originates from pancreatic alpha cells, resulting in overproduction of glucagon, which induces hyperglycemia, weight loss, and a characteristic rash called necrolytic migratory erythema. The fundamental pathophysiological difference lies in pheochromocytoma's catecholamine-driven sympathetic overstimulation versus glucagonoma's glucagon-induced metabolic dysregulation primarily affecting glucose metabolism.
Clinical Presentation and Symptoms
Pheochromocytoma typically presents with episodic hypertension, headaches, palpitations, and sweating due to excess catecholamine secretion. In contrast, Glucagonoma manifests with a characteristic migratory necrolytic erythema rash, weight loss, diabetes mellitus, and stomatitis linked to elevated glucagon levels. Both tumors exhibit distinct endocrine-related symptoms reflecting their neuroendocrine origins but require different diagnostic and therapeutic approaches.
Diagnostic Criteria and Biomarkers
Pheochromocytoma diagnosis relies on elevated plasma-free metanephrines and 24-hour urinary fractionated metanephrines, with imaging studies like MRI or CT confirming adrenal tumors. Glucagonoma detection centers on elevated fasting plasma glucagon levels, usually above 500 pg/mL, alongside clinical symptoms such as necrolytic migratory erythema and diabetes mellitus, supported by imaging to localize the pancreatic alpha-cell tumor. Both tumors require biochemical tests for hormone hypersecretion and advanced imaging for tumor localization, but their distinct biomarkers--metanephrines for pheochromocytoma and glucagon for glucagonoma--are key for differential diagnosis.
Imaging and Laboratory Investigations
Pheochromocytoma imaging primarily involves CT or MRI to detect adrenal tumors, alongside functional imaging with 123I-MIBG scintigraphy or PET scans using 18F-FDG or 18F-DOPA for localization and metastatic evaluation. Laboratory investigations focus on elevated plasma and urinary catecholamines or metanephrines, which serve as definitive biochemical markers. In contrast, glucagonoma diagnosis relies on contrast-enhanced CT or MRI for pancreatic mass identification, with laboratory results showing elevated plasma glucagon levels and a characteristic hyperglycemia profile.
Treatment and Management Approaches
Pheochromocytoma treatment primarily involves surgical resection of the adrenal tumor following preoperative management with alpha-adrenergic blockers to control hypertension and prevent intraoperative hypertensive crises. In contrast, glucagonoma management centers on surgical removal of the pancreatic neuroendocrine tumor, often supplemented by somatostatin analogs like octreotide to control hormone hypersecretion and manage symptoms such as necrolytic migratory erythema. Both conditions may require targeted therapies and symptomatic management, but pheochromocytoma emphasizes blood pressure stabilization while glucagonoma focuses on controlling glucagon excess.
Prognosis and Outcomes
Pheochromocytoma prognosis is generally favorable with timely surgical removal, boasting a 5-year survival rate exceeding 95%, although malignant cases may lead to metastasis and poorer outcomes. Glucagonoma prognosis depends heavily on early detection and tumor resection, with a median survival time of around 5 years for malignant cases due to metastatic potential and complications such as necrolytic migratory erythema. Both neuroendocrine tumors require careful management to improve long-term survival and minimize recurrence risks.
Complications and Associated Syndromes
Pheochromocytoma complications primarily include hypertensive crises, arrhythmias, and potential multi-organ damage due to excessive catecholamine secretion, often associating with genetic syndromes such as Multiple Endocrine Neoplasia type 2 (MEN 2) and Von Hippel-Lindau disease. Glucagonoma complications involve severe hyperglycemia, necrolytic migratory erythema, and thromboembolic events, frequently linked with Multiple Endocrine Neoplasia type 1 (MEN 1). Both tumors present significant systemic risks, but their biochemical profiles and related syndromes distinctly guide diagnosis and management.
Summary: Key Differences and Similarities
Pheochromocytoma is a rare adrenal medulla tumor characterized by excessive catecholamine secretion, causing hypertension, palpitations, and headaches, while glucagonoma is a pancreatic alpha-cell neuroendocrine tumor that secretes glucagon, leading to hyperglycemia and necrolytic migratory erythema. Both tumors originate from neuroendocrine cells and can cause paraneoplastic syndromes, but pheochromocytoma primarily affects the adrenal glands whereas glucagonoma arises in the pancreas. Diagnosis relies on biochemical tests measuring catecholamines for pheochromocytoma and elevated glucagon levels for glucagonoma, with imaging studies such as CT or MRI assisting localization.
Pheochromocytoma Infographic
 libterm.com
libterm.com