Apnea is a sleep disorder characterized by repeated interruptions in breathing during sleep, leading to fragmented rest and daytime fatigue. This condition can significantly impact your cardiovascular health and cognitive function if left untreated. Explore the article to understand apnea's symptoms, causes, and effective treatment options.
Table of Comparison
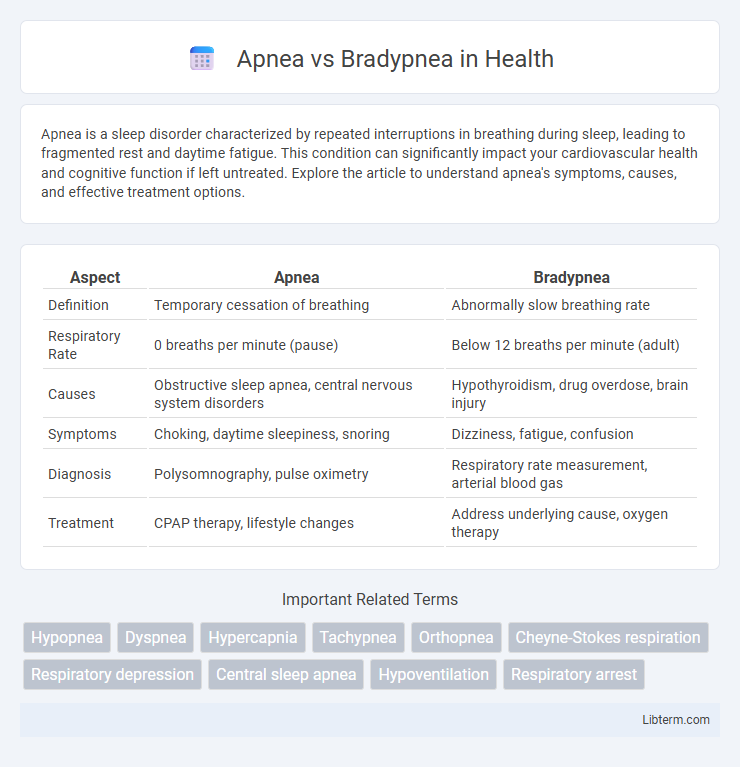
| Aspect | Apnea | Bradypnea |
|---|---|---|
| Definition | Temporary cessation of breathing | Abnormally slow breathing rate |
| Respiratory Rate | 0 breaths per minute (pause) | Below 12 breaths per minute (adult) |
| Causes | Obstructive sleep apnea, central nervous system disorders | Hypothyroidism, drug overdose, brain injury |
| Symptoms | Choking, daytime sleepiness, snoring | Dizziness, fatigue, confusion |
| Diagnosis | Polysomnography, pulse oximetry | Respiratory rate measurement, arterial blood gas |
| Treatment | CPAP therapy, lifestyle changes | Address underlying cause, oxygen therapy |
Understanding Apnea and Bradypnea: Key Definitions
Apnea is characterized by a complete cessation of airflow for at least 10 seconds during breathing, often linked to sleep disorders and respiratory failure. Bradypnea refers to an abnormally slow respiratory rate, typically fewer than 12 breaths per minute in adults, which can indicate neurological or metabolic conditions. Understanding these distinct respiratory dysfunctions is crucial for accurate diagnosis and treatment in clinical settings.
Causes of Apnea
Apnea occurs due to factors such as obstructive airway blockages, neurological disorders affecting the brainstem, and certain medications that suppress respiratory drive. Common causes include obstructive sleep apnea caused by relaxed throat muscles, central sleep apnea linked to impaired brain signaling, and drug-induced respiratory depression. Identifying these causes is crucial for effective diagnosis and treatment planning in respiratory care.
Causes of Bradypnea
Bradypnea, characterized by abnormally slow breathing rates below 12 breaths per minute in adults, can result from various causes such as drug overdose (opioids or sedatives), hypothyroidism, and neurological disorders including brain injury or stroke. Respiratory muscle weakness, often seen in conditions like myasthenia gravis or muscular dystrophy, also contributes to Bradypnea by impairing normal lung expansion. Chronic obstructive pulmonary disease (COPD) and electrolyte imbalances like hyperkalemia may further disrupt respiratory rhythm, leading to reduced respiratory rates distinctive of Bradypnea.
Symptoms Associated with Apnea vs Bradypnea
Apnea symptoms include sudden pauses in breathing, loud snoring, and excessive daytime sleepiness due to interrupted oxygen flow. Bradypnea symptoms consist of abnormally slow breathing, fatigue, dizziness, and confusion caused by insufficient oxygen intake. Both conditions require careful monitoring to prevent serious complications such as hypoxia or respiratory failure.
Risk Factors: Who is at Higher Risk?
Apnea risk factors primarily include obesity, smoking, and anatomical abnormalities such as enlarged tonsils or a deviated septum, with central apnea often linked to neurological disorders and heart failure. Bradypnea risk factors are commonly associated with underlying conditions like hypothyroidism, brain injury, or the use of certain medications that depress the respiratory center, including opioids and sedatives. Both conditions require careful assessment in patients with cardiovascular disease or neuromuscular disorders, as these populations are particularly vulnerable.
Diagnosing Apnea and Bradypnea
Diagnosing apnea involves monitoring for complete cessation of airflow for at least 10 seconds using polysomnography or overnight oximetry, which measures oxygen desaturation events. Bradypnea diagnosis emphasizes respiratory rate assessment, identifying abnormally slow breathing of fewer than 12 breaths per minute in adults through clinical observation or capnography. Accurate differentiation requires integrating respiratory pattern analysis with patient history and potential underlying conditions like sleep apnea or neurological disorders.
Complications and Health Risks
Apnea, characterized by temporary cessation of breathing, can lead to severe complications such as hypoxemia, cardiovascular disease, and increased risk of stroke due to prolonged oxygen deprivation. Bradypnea, defined by abnormally slow breathing rates, may cause inadequate ventilation resulting in elevated carbon dioxide levels and respiratory acidosis, potentially leading to organ dysfunction. Both conditions significantly compromise respiratory efficiency, increasing the risk of long-term health issues if untreated.
Treatment Approaches for Apnea
Treatment approaches for apnea primarily include continuous positive airway pressure (CPAP) therapy, which maintains open airways during sleep, and lifestyle modifications such as weight loss and avoiding alcohol or sedatives. In severe cases, surgical interventions like uvulopalatopharyngoplasty (UPPP) or hypoglossal nerve stimulation may be recommended to reduce airway obstruction. Management also involves addressing underlying conditions, monitoring oxygen levels, and utilizing oral appliances designed to reposition the jaw and tongue for improved airflow.
Treatment Approaches for Bradypnea
Treatment approaches for bradypnea primarily target the underlying cause, such as medication adjustments for opioid-induced respiratory depression or managing hypothyroidism with hormone replacement therapy. Mechanical ventilation or supplemental oxygen may be necessary in severe cases to maintain adequate oxygenation and carbon dioxide removal. Continuous monitoring of respiratory function is critical to tailor interventions and prevent complications related to insufficient breathing rates.
Preventive Measures and Lifestyle Modifications
Preventive measures for apnea and bradypnea emphasize maintaining a healthy weight, avoiding tobacco and alcohol use, and managing underlying medical conditions such as cardiovascular or pulmonary diseases. Lifestyle modifications include establishing regular sleep routines, practicing good sleep hygiene, and engaging in regular physical activity to improve respiratory function. In some cases, using continuous positive airway pressure (CPAP) devices or seeking medical evaluation for sleep disorders can effectively reduce the risk and severity of apneic episodes and abnormal breathing rates.
Apnea Infographic
 libterm.com
libterm.com