Ascites is the abnormal accumulation of fluid in the abdominal cavity, often caused by liver disease, cancer, or heart failure. Symptoms may include abdominal swelling, discomfort, and difficulty breathing, requiring prompt medical evaluation and treatment to manage underlying conditions. Discover more about the causes, symptoms, and treatment options for ascites in the remainder of this article.
Table of Comparison
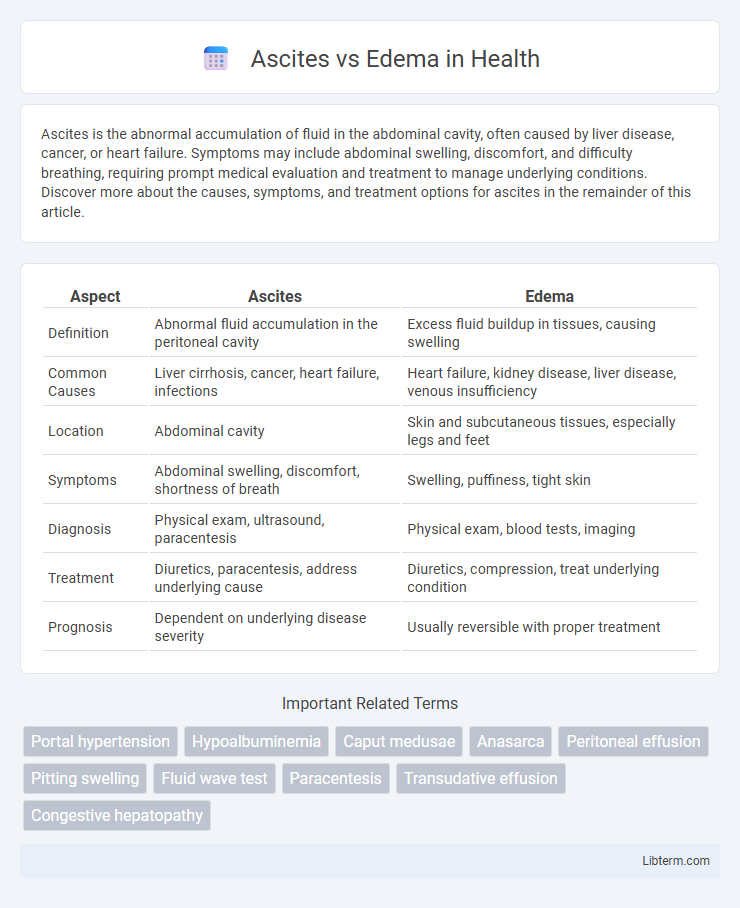
| Aspect | Ascites | Edema |
|---|---|---|
| Definition | Abnormal fluid accumulation in the peritoneal cavity | Excess fluid buildup in tissues, causing swelling |
| Common Causes | Liver cirrhosis, cancer, heart failure, infections | Heart failure, kidney disease, liver disease, venous insufficiency |
| Location | Abdominal cavity | Skin and subcutaneous tissues, especially legs and feet |
| Symptoms | Abdominal swelling, discomfort, shortness of breath | Swelling, puffiness, tight skin |
| Diagnosis | Physical exam, ultrasound, paracentesis | Physical exam, blood tests, imaging |
| Treatment | Diuretics, paracentesis, address underlying cause | Diuretics, compression, treat underlying condition |
| Prognosis | Dependent on underlying disease severity | Usually reversible with proper treatment |
Understanding Ascites and Edema: Key Differences
Ascites is the abnormal accumulation of fluid in the peritoneal cavity, often caused by liver cirrhosis, heart failure, or cancer. Edema refers to swelling caused by excess fluid trapped in the body's tissues, commonly found in the extremities and linked to conditions like kidney disease, venous insufficiency, or inflammation. Understanding these distinctions helps in diagnosing underlying causes and determining appropriate treatment strategies.
What Causes Ascites?
Ascites is primarily caused by liver cirrhosis, cancer, heart failure, or infections such as tuberculosis. Portal hypertension resulting from liver damage increases pressure in the blood vessels, leading to fluid accumulation in the abdominal cavity. Unlike peripheral edema, which involves fluid buildup in tissues, ascites specifically refers to fluid retention within the peritoneal cavity.
Common Causes of Edema
Edema commonly results from conditions such as congestive heart failure, chronic kidney disease, liver cirrhosis, and venous insufficiency, all of which disrupt fluid balance and cause excess fluid accumulation in tissues. Inflammatory reactions, malnutrition, and certain medications like calcium channel blockers can also trigger edema by increasing capillary permeability or impairing fluid removal. Understanding these causes helps differentiate edema from ascites, which specifically refers to fluid buildup in the peritoneal cavity largely caused by liver disease or malignancy.
Signs and Symptoms: Ascites vs Edema
Ascites presents as abdominal swelling, discomfort, and a feeling of fullness due to fluid accumulation in the peritoneal cavity, often accompanied by increased abdominal girth and shifting dullness on physical examination. Edema manifests as localized or generalized swelling, primarily in the lower extremities, hands, or face, with skin appearing stretched and shiny, and may leave a pitting mark when pressed due to interstitial fluid retention. Both conditions indicate fluid imbalance but differ in fluid location and associated signs such as bulging flanks and fluid wave in ascites versus dependent limb swelling in edema.
Physical Examination Findings
Ascites is characterized by abdominal distension with fluid wave and shifting dullness on percussion, indicating free fluid in the peritoneal cavity, whereas edema presents as pitting swelling mainly in dependent areas such as the lower extremities. In ascites, inspection reveals a tense, bulging abdomen, and on palpation, fluid thrill may be detected, contrasting with edema's soft, boggy texture without localized fluid accumulation. Auscultation in ascites often shows diminished bowel sounds due to fluid displacement, while in edema, pulmonary auscultation may reveal signs of fluid overload such as crackles if associated with cardiac causes.
Diagnostic Approaches for Ascites
Diagnostic approaches for ascites primarily include physical examination techniques like shifting dullness and fluid wave tests to detect abnormal abdominal fluid accumulation. Ultrasound imaging serves as a highly sensitive tool to confirm ascitic fluid presence, guide paracentesis, and evaluate underlying causes such as liver cirrhosis or malignancy. Analysis of ascitic fluid obtained through paracentesis, including cell count, albumin, and culture, remains essential for distinguishing between transudative and exudative ascites, informing targeted treatment strategies.
Diagnostic Approaches for Edema
Diagnostic approaches for edema primarily involve a thorough clinical examination combined with laboratory tests such as serum albumin, renal function, and electrolytes to identify underlying causes like heart, liver, or kidney disease. Imaging techniques, including ultrasound and echocardiography, assist in assessing fluid accumulation and organ function, while Doppler studies help evaluate venous insufficiency or thrombosis. Biomarkers like B-type natriuretic peptide (BNP) levels provide additional insights into cardiac-related edema, enhancing diagnostic accuracy.
Treatment Strategies: Ascites
Treatment strategies for ascites primarily involve sodium restriction and diuretic therapy using agents like spironolactone and furosemide to promote fluid removal. Paracentesis is an effective procedure for large or refractory ascites, providing symptomatic relief by physically draining excess fluid from the peritoneal cavity. In cases of cirrhosis-related ascites, managing the underlying liver disease, including considering transjugular intrahepatic portosystemic shunt (TIPS) placement, enhances treatment outcomes and reduces fluid accumulation.
Treatment Strategies: Edema
Treatment strategies for edema primarily involve addressing the underlying cause, such as heart failure, kidney disease, or venous insufficiency, alongside symptomatic management. Diuretics like furosemide help reduce fluid accumulation by increasing urine output, while compression therapy promotes venous return and decreases swelling. Lifestyle modifications including salt restriction, leg elevation, and regular physical activity support long-term edema control and prevent recurrence.
Prognosis and Long-Term Management
Ascites, characterized by the accumulation of fluid in the peritoneal cavity, often indicates advanced liver disease or malignancy, with prognosis heavily dependent on the underlying cause and response to therapies such as diuretics and paracentesis. Edema, involving widespread interstitial fluid retention typically due to heart failure, kidney disease, or venous insufficiency, requires targeted management of these conditions to improve outcomes and reduce recurrence risk. Long-term management for ascites emphasizes controlling portal hypertension and preventing complications like spontaneous bacterial peritonitis, while edema management focuses on lifestyle modifications, medication adherence, and treating the primary disorder to enhance quality of life.
Ascites Infographic
 libterm.com
libterm.com