Hyperphosphatemia occurs when there is an abnormally high level of phosphate in the blood, often linked to kidney dysfunction or excessive dietary phosphate intake. This condition can lead to serious complications such as vascular calcification and cardiovascular disease if left untreated. Discover how you can manage hyperphosphatemia effectively and protect your overall health by reading the full article.
Table of Comparison
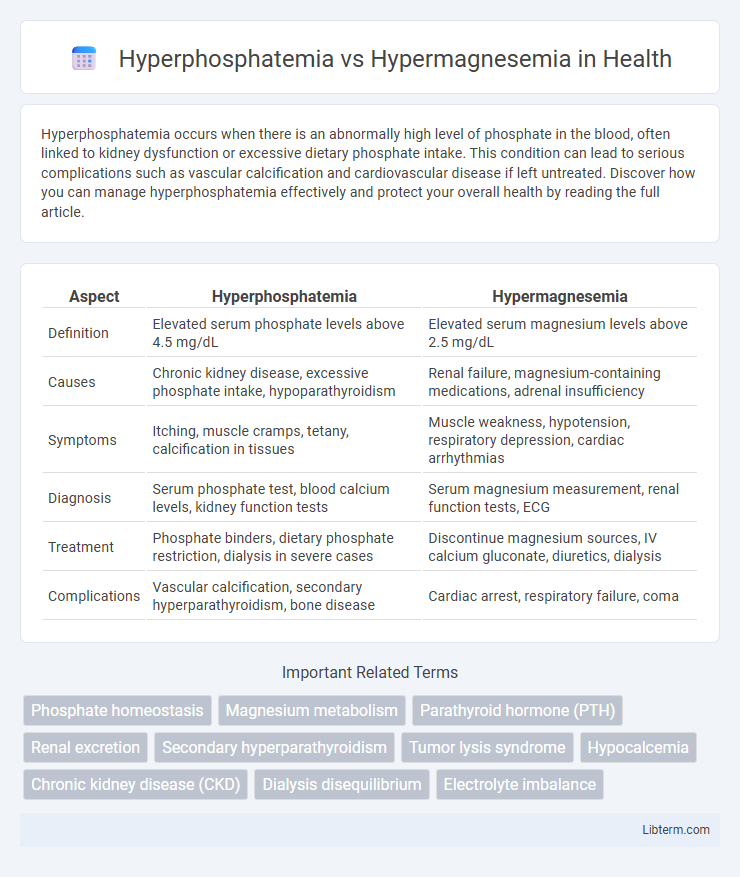
| Aspect | Hyperphosphatemia | Hypermagnesemia |
|---|---|---|
| Definition | Elevated serum phosphate levels above 4.5 mg/dL | Elevated serum magnesium levels above 2.5 mg/dL |
| Causes | Chronic kidney disease, excessive phosphate intake, hypoparathyroidism | Renal failure, magnesium-containing medications, adrenal insufficiency |
| Symptoms | Itching, muscle cramps, tetany, calcification in tissues | Muscle weakness, hypotension, respiratory depression, cardiac arrhythmias |
| Diagnosis | Serum phosphate test, blood calcium levels, kidney function tests | Serum magnesium measurement, renal function tests, ECG |
| Treatment | Phosphate binders, dietary phosphate restriction, dialysis in severe cases | Discontinue magnesium sources, IV calcium gluconate, diuretics, dialysis |
| Complications | Vascular calcification, secondary hyperparathyroidism, bone disease | Cardiac arrest, respiratory failure, coma |
Introduction to Hyperphosphatemia and Hypermagnesemia
Hyperphosphatemia, characterized by elevated serum phosphate levels exceeding 4.5 mg/dL, commonly results from chronic kidney disease or hypoparathyroidism, leading to vascular calcification and disrupted mineral metabolism. Hypermagnesemia, defined by magnesium concentrations above 2.5 mg/dL, often arises from renal insufficiency or excessive magnesium intake, causing neuromuscular and cardiovascular complications. Both electrolyte imbalances require accurate diagnosis and targeted management to mitigate systemic toxicity and organ dysfunction.
Causes of Hyperphosphatemia
Hyperphosphatemia primarily results from renal failure, where impaired kidney function reduces phosphate excretion, leading to elevated serum phosphate levels. Other causes include excessive phosphate intake, hypoparathyroidism, and cellular breakdown such as in tumor lysis syndrome or rhabdomyolysis. Unlike hypermagnesemia, which is commonly caused by magnesium supplementation, renal dysfunction, or antacid overuse, hyperphosphatemia specifically reflects disturbances in phosphate metabolism related to kidney impairment and metabolic imbalances.
Causes of Hypermagnesemia
Hypermagnesemia is primarily caused by excessive magnesium intake, often due to overuse of magnesium-containing laxatives or antacids, especially in patients with renal insufficiency who cannot efficiently excrete magnesium. Other causes include adrenal insufficiency, hypothyroidism, and severe tissue breakdown such as in rhabdomyolysis or tumor lysis syndrome. In contrast, hyperphosphatemia mainly results from chronic kidney disease, hypoparathyroidism, or increased phosphate load from tumor lysis or rhabdomyolysis.
Clinical Signs and Symptoms: Hyperphosphatemia
Hyperphosphatemia often manifests with clinical signs such as muscle cramps, tetany, and paresthesia due to calcium-phosphate imbalances. Patients may also experience symptoms related to secondary hypocalcemia, including numbness around the mouth and extremities, as well as potential cardiac arrhythmias. Chronic hyperphosphatemia can contribute to vascular calcification and soft tissue calcification, exacerbating cardiovascular risks.
Clinical Signs and Symptoms: Hypermagnesemia
Hypermagnesemia commonly presents with muscle weakness, hypotension, and respiratory depression due to neuromuscular blockade, whereas hyperphosphatemia often manifests with symptoms related to secondary hypocalcemia such as tetany and muscle cramps. Elevated serum magnesium levels can cause diminished deep tendon reflexes, confusion, and cardiac arrhythmias including bradycardia and heart block. In severe cases, hypermagnesemia may lead to coma or cardiac arrest if not promptly treated.
Pathophysiological Differences
Hyperphosphatemia arises from impaired renal phosphate excretion or excessive phosphate load, leading to elevated serum phosphate levels that promote calcium-phosphate complex deposition and subsequent tissue calcification. In contrast, hypermagnesemia results from reduced renal magnesium clearance or excessive magnesium intake, causing increased serum magnesium that depresses neuromuscular excitability and cardiac conduction. The key pathophysiological distinction lies in hyperphosphatemia's impact on mineral metabolism and soft tissue calcification versus hypermagnesemia's effect on neuromuscular and cardiovascular function.
Diagnostic Approaches
Diagnostic approaches for hyperphosphatemia involve measuring serum phosphate levels, assessing kidney function through blood urea nitrogen and creatinine tests, and evaluating parathyroid hormone (PTH) levels to identify underlying causes such as chronic kidney disease or hypoparathyroidism. In hypermagnesemia, diagnosis includes serum magnesium concentration analysis, often alongside renal function tests and evaluation of medication history (e.g., magnesium-containing laxatives or antacids), to detect impaired renal excretion or excessive magnesium intake. Both conditions require careful interpretation of electrolyte panels combined with clinical assessment to guide appropriate management strategies.
Management Strategies: Hyperphosphatemia
Management strategies for hyperphosphatemia primarily involve dietary phosphate restriction and the use of phosphate binders such as sevelamer or calcium acetate to reduce serum phosphate levels. Dialysis is often required in patients with chronic kidney disease to effectively remove excess phosphate from the bloodstream. Controlling hyperphosphatemia is crucial to prevent complications like vascular calcification and secondary hyperparathyroidism.
Management Strategies: Hypermagnesemia
Management strategies for hypermagnesemia primarily involve intravenous calcium gluconate to counteract neuromuscular and cardiovascular effects, along with discontinuation of magnesium-containing medications and supplements. In severe cases, especially when renal function is impaired, emergency hemodialysis effectively reduces serum magnesium levels. Diuretics and hydration may be used to enhance renal magnesium excretion in patients with preserved kidney function.
Prevention and Prognosis
Effective prevention of hyperphosphatemia involves dietary phosphate restriction and the use of phosphate binders, particularly in patients with chronic kidney disease, while hypermagnesemia prevention centers on monitoring magnesium intake and avoiding magnesium-containing medications in susceptible individuals. Prognosis for hyperphosphatemia remains guarded due to its association with vascular calcification and cardiovascular morbidity, whereas hypermagnesemia prognosis varies with severity but generally improves with prompt discontinuation of magnesium sources and supportive treatments such as calcium administration and dialysis. Early intervention and regular biochemical monitoring are crucial for improving outcomes and preventing complications in both conditions.
Hyperphosphatemia Infographic
 libterm.com
libterm.com