Hemorrhage refers to the escape of blood from a ruptured blood vessel, leading to internal or external bleeding that can vary in severity. Prompt recognition and treatment are critical to prevent complications such as shock or organ failure. Explore the full article to understand the types, causes, and effective management strategies for hemorrhage.
Table of Comparison
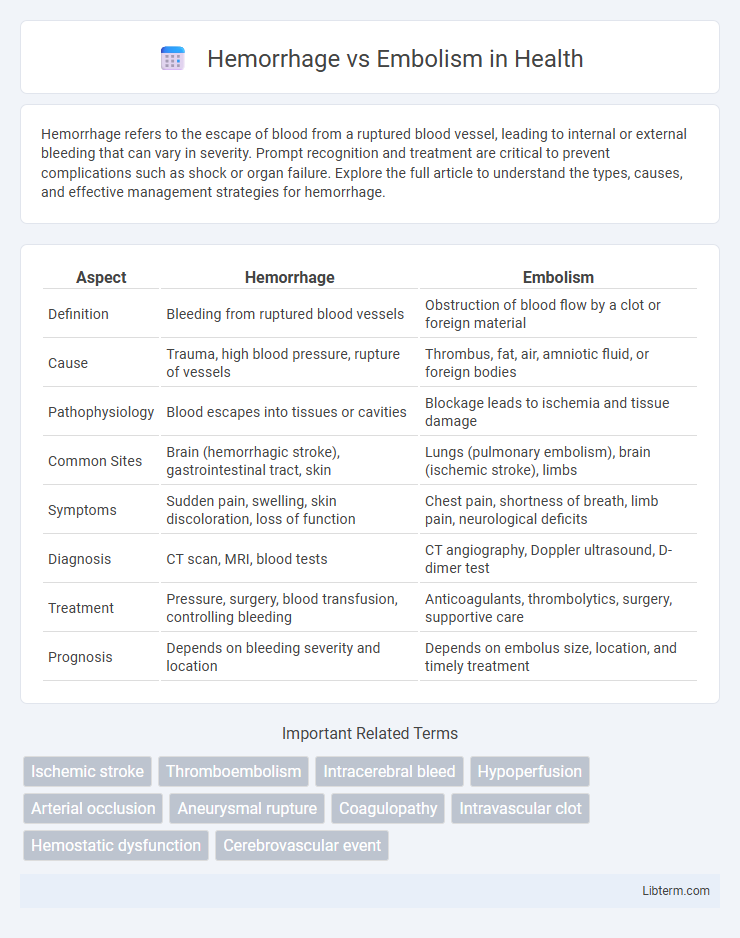
| Aspect | Hemorrhage | Embolism |
|---|---|---|
| Definition | Bleeding from ruptured blood vessels | Obstruction of blood flow by a clot or foreign material |
| Cause | Trauma, high blood pressure, rupture of vessels | Thrombus, fat, air, amniotic fluid, or foreign bodies |
| Pathophysiology | Blood escapes into tissues or cavities | Blockage leads to ischemia and tissue damage |
| Common Sites | Brain (hemorrhagic stroke), gastrointestinal tract, skin | Lungs (pulmonary embolism), brain (ischemic stroke), limbs |
| Symptoms | Sudden pain, swelling, skin discoloration, loss of function | Chest pain, shortness of breath, limb pain, neurological deficits |
| Diagnosis | CT scan, MRI, blood tests | CT angiography, Doppler ultrasound, D-dimer test |
| Treatment | Pressure, surgery, blood transfusion, controlling bleeding | Anticoagulants, thrombolytics, surgery, supportive care |
| Prognosis | Depends on bleeding severity and location | Depends on embolus size, location, and timely treatment |
Understanding Hemorrhage: Definition and Causes
Hemorrhage refers to the excessive or uncontrolled bleeding caused by the rupture of blood vessels, leading to blood escaping into surrounding tissues or body cavities. Common causes of hemorrhage include trauma, hypertension, aneurysms, and certain medical conditions like hemophilia or vascular malformations. Understanding the pathophysiology of hemorrhage is crucial for diagnosing conditions such as intracranial hemorrhage or gastrointestinal bleeding and implementing timely medical interventions.
What Is an Embolism? Types and Risk Factors
An embolism occurs when a blood clot, air bubble, fat globule, or other substance blocks a blood vessel, disrupting normal blood flow. The primary types of embolism include pulmonary embolism, arterial embolism, fat embolism, air embolism, and septic embolism, each differing by the material causing the blockage and its location. Risk factors for embolism include prolonged immobility, recent surgery, certain medical conditions like atrial fibrillation, deep vein thrombosis, smoking, obesity, and genetic clotting disorders.
Key Differences Between Hemorrhage and Embolism
Hemorrhage is the uncontrolled bleeding caused by blood vessel rupture, resulting in blood escaping into surrounding tissues, whereas embolism refers to the obstruction of a blood vessel by a clot, air bubble, fat globule, or other foreign material traveling through the bloodstream. Hemorrhage leads to local tissue damage due to blood loss and pressure, while embolism causes ischemia and potential infarction by blocking blood flow. Treatment strategies differ significantly: hemorrhage requires bleeding control and volume replacement, whereas embolism demands restoring vessel patency and preventing further clot migration.
Signs and Symptoms of Hemorrhage
Hemorrhage presents with signs such as rapid swelling, intense pain, and visible bleeding from the affected area, alongside symptoms like dizziness, weakness, and pallor due to significant blood loss. Internal hemorrhages might cause localized tenderness, a rapid drop in blood pressure, and confusion or loss of consciousness in severe cases. Early detection of these signs is critical to differentiate hemorrhage from embolism, which typically manifests with sudden obstruction symptoms without external bleeding.
Clinical Presentation of Embolism
Embolism typically presents with sudden onset of symptoms such as acute pain, pallor, pulselessness, and paralysis in the affected limb, reflecting arterial occlusion. Patients often experience rapid ischemia leading to tissue hypoxia, which can cause neurological deficits if cerebral vessels are involved. Timely diagnosis is critical, relying on clinical signs combined with imaging modalities like Doppler ultrasound or CT angiography to confirm the embolic event.
Diagnostic Approaches for Hemorrhage vs Embolism
Diagnostic approaches for hemorrhage primarily include imaging techniques such as computed tomography (CT) scans and magnetic resonance imaging (MRI) to identify bleeding sites and assess hemorrhage extent. Embolism diagnosis relies heavily on Doppler ultrasound, CT pulmonary angiography, and echocardiography to detect occlusions within blood vessels and evaluate blood flow disruptions. Laboratory tests, including coagulation profiles and D-dimer levels, complement imaging studies by providing information on bleeding risk and thrombus presence, distinguishing hemorrhage from embolic events.
Treatment Strategies for Hemorrhage
Treatment strategies for hemorrhage prioritize rapid hemostasis using techniques such as direct pressure application, surgical ligation, or embolization with agents like coils or particles to control bleeding. Fluid resuscitation with crystalloids and blood transfusions are critical to restore circulating volume and prevent shock. Advanced interventions might include administration of clotting factors and reversal of anticoagulant medications to stabilize hemostasis effectively.
Management of Embolic Events
Management of embolic events focuses on rapid identification and prompt intervention to restore blood flow and minimize tissue damage. Anticoagulant therapy, such as heparin or warfarin, is essential to prevent clot propagation, while thrombolytic agents may be used in severe cases to dissolve emboli. Surgical or catheter-based embolectomy is considered when pharmacological treatment is contraindicated or ineffective, ensuring timely reperfusion in critical embolic occlusions.
Preventive Measures for Hemorrhage and Embolism
Preventive measures for hemorrhage include controlling hypertension, avoiding anticoagulant overdose, and maintaining vascular health through a balanced diet rich in vitamin K and regular exercise. Embolism prevention focuses on managing risk factors such as atrial fibrillation, deep vein thrombosis, and prolonged immobility by using anticoagulants, compression stockings, and early mobilization after surgery. Both conditions benefit from routine medical monitoring, prompt treatment of related cardiovascular diseases, and lifestyle modifications to reduce clot formation and vessel rupture risks.
Prognosis and Long-term Outcomes
Hemorrhage typically results in localized brain damage with prognosis depending on the hemorrhage size and location, often leading to significant neurological deficits and increased mortality risk. Embolism, causing ischemic strokes, varies in outcome based on the embolus origin and timely reperfusion, with many patients achieving partial to full recovery through early intervention and rehabilitation. Long-term outcomes for both conditions include the potential for recurrent events, necessitating ongoing management of underlying risk factors like hypertension, atrial fibrillation, and vascular disease.
Hemorrhage Infographic
 libterm.com
libterm.com