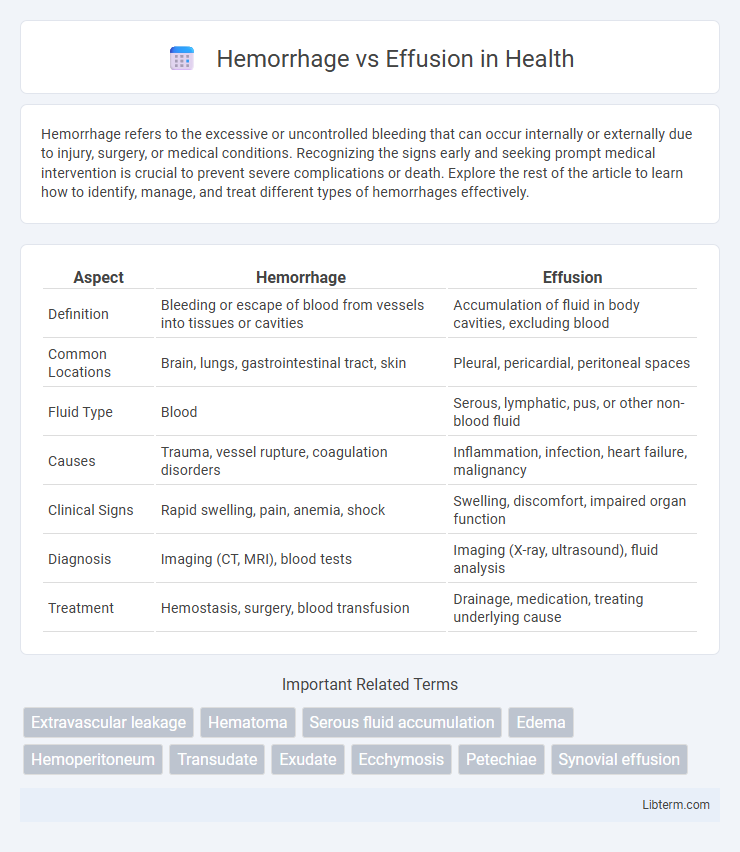
Hemorrhage refers to the excessive or uncontrolled bleeding that can occur internally or externally due to injury, surgery, or medical conditions. Recognizing the signs early and seeking prompt medical intervention is crucial to prevent severe complications or death. Explore the rest of the article to learn how to identify, manage, and treat different types of hemorrhages effectively.
Table of Comparison
| Aspect | Hemorrhage | Effusion |
|---|---|---|
| Definition | Bleeding or escape of blood from vessels into tissues or cavities | Accumulation of fluid in body cavities, excluding blood |
| Common Locations | Brain, lungs, gastrointestinal tract, skin | Pleural, pericardial, peritoneal spaces |
| Fluid Type | Blood | Serous, lymphatic, pus, or other non-blood fluid |
| Causes | Trauma, vessel rupture, coagulation disorders | Inflammation, infection, heart failure, malignancy |
| Clinical Signs | Rapid swelling, pain, anemia, shock | Swelling, discomfort, impaired organ function |
| Diagnosis | Imaging (CT, MRI), blood tests | Imaging (X-ray, ultrasound), fluid analysis |
| Treatment | Hemostasis, surgery, blood transfusion | Drainage, medication, treating underlying cause |
Understanding Hemorrhage: Definition and Causes
Hemorrhage refers to the abnormal or excessive bleeding caused by the rupture of blood vessels, leading to blood escaping into surrounding tissues or body cavities. Common causes include trauma, hypertension, blood clotting disorders, and vascular diseases, which can result in internal or external bleeding. Understanding the mechanisms and origins of hemorrhage is crucial for accurate diagnosis and effective medical intervention.
What is an Effusion? Types and Triggers
An effusion is the abnormal accumulation of fluid within a body cavity, commonly occurring in the pleural, pericardial, or peritoneal spaces. Types of effusions include transudative, caused by systemic factors like congestive heart failure or hypoalbuminemia, and exudative, resulting from local inflammation or infection such as pneumonia or malignancy. Triggers for effusions often involve trauma, infection, malignancy, or chronic diseases, leading to fluid leakage due to increased vascular permeability or impaired fluid drainage.
Key Differences Between Hemorrhage and Effusion
Hemorrhage involves active bleeding caused by ruptured blood vessels leading to blood accumulation outside the circulatory system, whereas effusion refers to fluid buildup in body cavities due to inflammation, infection, or injury without active bleeding. Hemorrhages are characterized by the presence of fresh or clotted blood, while effusions contain serous, purulent, or chylous fluid depending on the underlying condition. Diagnostic methods differ, with imaging and fluid analysis helping distinguish hemorrhagic blood from non-bloody effusions for appropriate clinical management.
Clinical Presentation: Signs and Symptoms
Hemorrhage often presents with sudden, severe pain, swelling, and visible bruising or hematoma, indicating active bleeding into tissues or cavities. Effusion typically manifests as joint swelling, warmth, and restricted movement due to fluid accumulation, with symptoms progressing more gradually than hemorrhage. Both conditions require thorough clinical evaluation to distinguish the source of fluid and associated systemic signs such as fever or drop in hemoglobin in hemorrhage cases.
Diagnostic Techniques: Hemorrhage vs. Effusion
Diagnostic techniques for hemorrhage often involve imaging modalities such as CT scans and MRI to identify blood accumulation and its source, while ultrasound is valuable in detecting effusions by visualizing fluid in cavities like the pleura or peritoneum. Laboratory analysis of aspirated fluid differentiates hemorrhage from effusion through assessment of red blood cell count, hemoglobin concentration, and biochemical markers such as protein levels and lactate dehydrogenase. Advanced diagnostics include Doppler ultrasound to evaluate vascular integrity in hemorrhage cases and cytological examination to determine the nature of effusion, distinguishing between transudates and exudates.
Common Locations and Associated Conditions
Hemorrhages commonly occur in the brain (intracranial hemorrhage), gastrointestinal tract, and muscles, often linked to trauma, hypertension, or coagulation disorders. Effusions typically accumulate in body cavities such as the pleural space (pleural effusion), peritoneal cavity (ascites), and pericardial sac (pericardial effusion), frequently associated with infections, malignancies, or inflammatory conditions. Differentiating these is crucial in clinical diagnosis, as hemorrhage signifies active bleeding, while effusion involves fluid buildup without vessel rupture.
Treatment Approaches for Hemorrhage
Treatment approaches for hemorrhage prioritize rapid stabilization of the patient through fluid resuscitation and blood transfusions to restore hemodynamic stability. Surgical intervention or endovascular techniques may be required to control the bleeding source, especially in cases of severe trauma or ruptured vessels. Medications such as antifibrinolytics can help reduce bleeding by promoting clot formation, while continuous monitoring ensures timely adjustments in therapy.
Management Strategies for Effusion
Management strategies for effusion focus on accurate diagnosis through imaging techniques such as ultrasound or MRI to determine the underlying cause. Treatment typically involves aspiration to relieve symptoms and prevent complications, combined with addressing the root etiology, such as infection, inflammation, or malignancy. In some cases, long-term management includes the use of corticosteroids, antibiotics, or surgical interventions like pleurodesis to prevent recurrence.
Complications and Prognosis
Hemorrhage, characterized by active bleeding, can lead to complications such as hypovolemic shock, organ damage, and increased intracranial pressure, worsening patient prognosis if untreated. Effusion involves abnormal fluid accumulation in body cavities, potentially causing impaired organ function, infection, or fibrosis, which can complicate recovery depending on the effusion's location and cause. Prognosis varies widely; hemorrhages often require urgent intervention with risk of morbidity, while effusions may resolve with treatment but can signal chronic underlying conditions affecting long-term outcomes.
Prevention and Monitoring Tips
Preventing hemorrhage involves controlling risk factors such as hypertension and avoiding anticoagulant misuse, while effusion prevention focuses on managing underlying conditions like heart failure or infections. Regular monitoring through imaging techniques like ultrasound or CT scans and routine blood tests helps detect early signs of bleeding or fluid accumulation. Prompt medical evaluation of symptoms such as sudden pain, swelling, or respiratory distress is crucial to prevent complications from both hemorrhage and effusion.
Hemorrhage Infographic
 libterm.com
libterm.com