Pleomorphic adenoma is the most common benign tumor of the salivary glands, characterized by its mixed cellular composition and slow growth. Early diagnosis and appropriate surgical removal are crucial to prevent recurrence and potential malignant transformation. Explore the full article to understand the symptoms, treatment options, and long-term management of this condition.
Table of Comparison
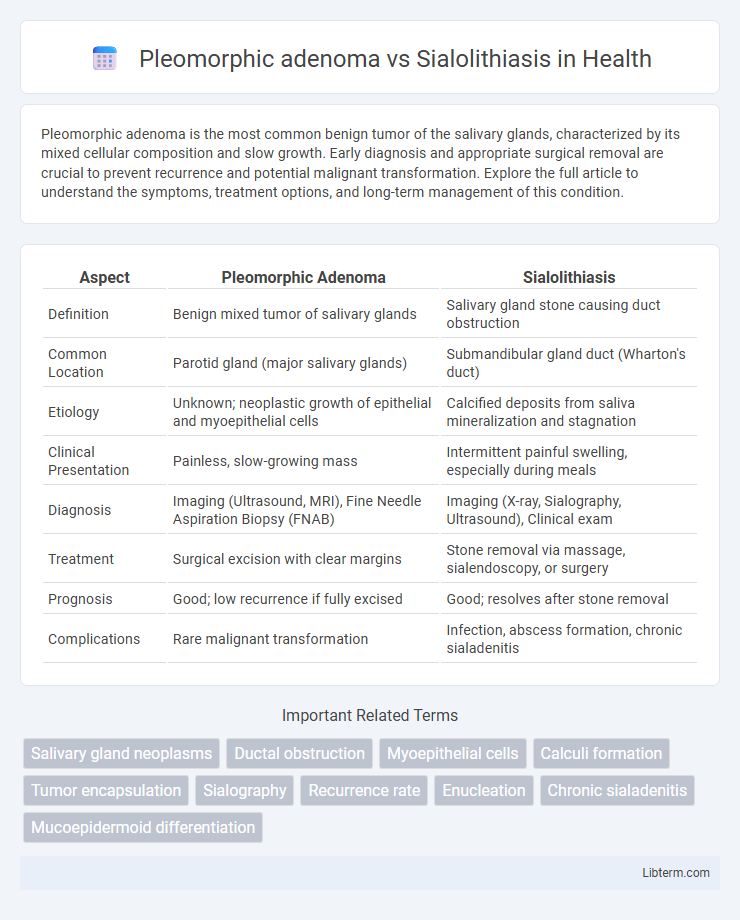
| Aspect | Pleomorphic Adenoma | Sialolithiasis |
|---|---|---|
| Definition | Benign mixed tumor of salivary glands | Salivary gland stone causing duct obstruction |
| Common Location | Parotid gland (major salivary glands) | Submandibular gland duct (Wharton's duct) |
| Etiology | Unknown; neoplastic growth of epithelial and myoepithelial cells | Calcified deposits from saliva mineralization and stagnation |
| Clinical Presentation | Painless, slow-growing mass | Intermittent painful swelling, especially during meals |
| Diagnosis | Imaging (Ultrasound, MRI), Fine Needle Aspiration Biopsy (FNAB) | Imaging (X-ray, Sialography, Ultrasound), Clinical exam |
| Treatment | Surgical excision with clear margins | Stone removal via massage, sialendoscopy, or surgery |
| Prognosis | Good; low recurrence if fully excised | Good; resolves after stone removal |
| Complications | Rare malignant transformation | Infection, abscess formation, chronic sialadenitis |
Introduction to Pleomorphic Adenoma and Sialolithiasis
Pleomorphic adenoma, the most common benign salivary gland tumor, primarily affects the parotid gland and presents as a slow-growing, painless mass. Sialolithiasis involves the formation of calcified stones within the salivary ducts, typically causing acute pain and swelling due to obstruction, most frequently in the submandibular gland. Both conditions impact salivary gland function but differ in etiology and clinical presentation.
Overview of Salivary Gland Diseases
Pleomorphic adenoma is the most common benign salivary gland tumor characterized by a mixed epithelial and myoepithelial cell origin, typically presenting as a painless, slow-growing mass in the parotid gland. Sialolithiasis involves the formation of calcified stones obstructing the salivary ducts, leading to painful swelling and possible infection, most frequently affecting the submandibular gland. Both conditions represent common salivary gland diseases but differ significantly in etiology, clinical presentation, and management strategies.
Etiology: Causes of Pleomorphic Adenoma vs. Sialolithiasis
Pleomorphic adenoma originates primarily from the myoepithelial and ductal cells of salivary glands due to genetic abnormalities such as PLAG1 and HMGA2 gene rearrangements, contributing to its benign tumor development. Sialolithiasis is caused by the formation of calcified stones within salivary gland ducts, often triggered by factors like reduced salivary flow, dehydration, altered saliva composition, and chronic inflammation. Distinguishing these etiologies helps in understanding the benign neoplastic growth of pleomorphic adenoma versus the obstructive and inflammatory nature of sialolithiasis.
Pathophysiology: Structural and Functional Changes
Pleomorphic adenoma is characterized by the proliferation of both epithelial and myoepithelial cells forming a mixed tumor with a chondromyxoid stroma, leading to slow, painless glandular enlargement primarily affecting the parotid gland. Sialolithiasis involves the formation of calcified salivary gland stones within the ducts, causing mechanical obstruction that leads to ductal dilatation, increased intraductal pressure, and inflammation, often resulting in painful swelling during salivation. The structural changes in pleomorphic adenoma reflect neoplastic growth with preserved gland architecture, whereas sialolithiasis induces functional impairment through obstructive phenomena and secondary inflammatory damage.
Clinical Presentation and Symptoms
Pleomorphic adenoma typically presents as a slow-growing, painless, firm mass in the parotid or other salivary glands, often without signs of infection or inflammation. Sialolithiasis, characterized by salivary gland duct stones, commonly causes intermittent pain and swelling in the affected gland, especially during meals, accompanied by possible gland tenderness and erythema. Unlike pleomorphic adenoma, sialolithiasis symptoms often include acute episodes of obstruction leading to glandular infection or abscess formation.
Diagnostic Approaches and Imaging Techniques
Pleomorphic adenoma diagnosis often involves ultrasound imaging combined with fine-needle aspiration cytology to differentiate benign from malignant salivary gland tumors, with MRI providing detailed soft tissue contrast for tumor margins. In contrast, sialolithiasis is primarily identified through non-contrast computed tomography (CT) scans, which effectively detect calcified salivary stones, while ultrasound can reveal ductal dilation and stone presence. Both conditions benefit from sialography in complex cases, aiding visualization of salivary duct obstructions versus solid masses.
Histopathological Differences
Pleomorphic adenoma histopathology reveals a well-circumscribed tumor with a mixture of epithelial and myoepithelial cells embedded in a chondromyxoid stroma, exhibiting ductal structures and a myxoid or chondroid matrix. Sialolithiasis histopathology shows ductal obstruction with associated chronic inflammation, ductal epithelial hyperplasia, and periductal fibrosis, without tumor formation. The presence of a neoplastic biphasic cell population distinguishes pleomorphic adenoma from the inflammatory changes and stone-induced damage characteristic of sialolithiasis.
Treatment Options and Patient Management
Pleomorphic adenoma primarily requires surgical excision with a margin of healthy tissue to prevent recurrence and malignant transformation, while sialolithiasis treatment ranges from conservative management with hydration and massage to minimally invasive sialendoscopy or surgical removal of the obstructing stone. Patient management for pleomorphic adenoma involves regular follow-up imaging to monitor for recurrence, whereas sialolithiasis often necessitates symptomatic relief and infection control, with periodic evaluation to detect residual stones or ductal damage. Postoperative care differs significantly, emphasizing surveillance and early intervention in pleomorphic adenoma and functional restoration with ductal patency in sialolithiasis.
Prognosis, Recurrence, and Complications
Pleomorphic adenoma, a benign salivary gland tumor, often has an excellent prognosis with low malignant transformation risk but requires complete excision due to a recurrence rate of up to 5-10% if not fully removed. Sialolithiasis, characterized by salivary gland duct stones, generally resolves with conservative or surgical treatment, posing minimal long-term complications but may lead to gland infection or chronic sialadenitis if untreated. Both conditions entail potential complications, but pleomorphic adenoma's risk of recurrence and malignant transformation makes thorough surgical management critical for optimal outcomes.
Key Differences and Summary Comparison
Pleomorphic adenoma is a benign salivary gland tumor characterized by a mixed cellular composition, slow growth, and painless swelling, typically affecting the parotid gland. Sialolithiasis involves the formation of calcified stones within the salivary ducts, leading to painful obstruction, swelling, and sometimes infection, commonly in the submandibular gland. Key differences include etiology, with pleomorphic adenoma arising from glandular tissue proliferation versus sialolithiasis caused by ductal obstruction from calculi, as well as clinical presentation, diagnostic imaging features, and management strategies.
Pleomorphic adenoma Infographic
 libterm.com
libterm.com