Hypophosphatemia is a condition characterized by abnormally low levels of phosphate in the blood, which can lead to muscle weakness, bone pain, and impaired cellular function. Identifying the underlying causes, such as malnutrition, chronic alcoholism, or certain medications, is crucial for effective treatment. Explore the rest of the article to understand the symptoms, diagnosis, and management options for hypophosphatemia and how it may affect your health.
Table of Comparison
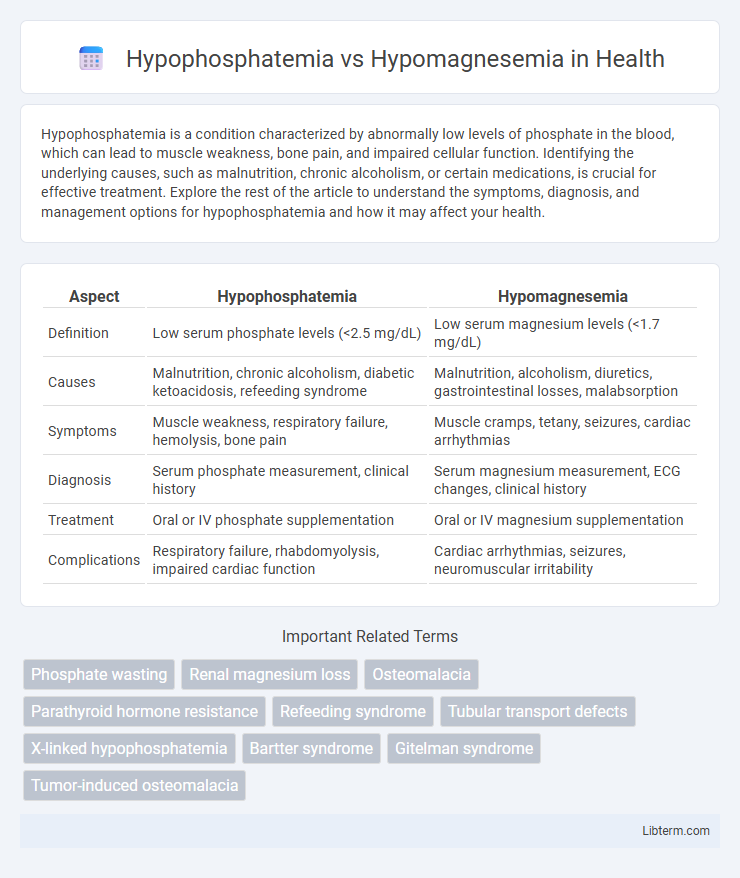
| Aspect | Hypophosphatemia | Hypomagnesemia |
|---|---|---|
| Definition | Low serum phosphate levels (<2.5 mg/dL) | Low serum magnesium levels (<1.7 mg/dL) |
| Causes | Malnutrition, chronic alcoholism, diabetic ketoacidosis, refeeding syndrome | Malnutrition, alcoholism, diuretics, gastrointestinal losses, malabsorption |
| Symptoms | Muscle weakness, respiratory failure, hemolysis, bone pain | Muscle cramps, tetany, seizures, cardiac arrhythmias |
| Diagnosis | Serum phosphate measurement, clinical history | Serum magnesium measurement, ECG changes, clinical history |
| Treatment | Oral or IV phosphate supplementation | Oral or IV magnesium supplementation |
| Complications | Respiratory failure, rhabdomyolysis, impaired cardiac function | Cardiac arrhythmias, seizures, neuromuscular irritability |
Introduction to Hypophosphatemia and Hypomagnesemia
Hypophosphatemia is characterized by abnormally low serum phosphate levels, typically below 2.5 mg/dL, disrupting cellular energy metabolism and bone mineralization. Hypomagnesemia involves reduced serum magnesium concentrations, generally under 1.7 mg/dL, impairing neuromuscular function and cardiovascular stability. Both electrolyte imbalances often result from malnutrition, renal disorders, or chronic alcoholism, requiring precise biochemical assessment for accurate diagnosis and management.
Definitions and Key Differences
Hypophosphatemia is characterized by abnormally low levels of phosphate in the blood, essential for cellular energy and bone formation, whereas hypomagnesemia involves a deficiency of magnesium, a critical mineral for enzyme function and neuromuscular stability. The primary difference lies in their metabolic roles: phosphate predominantly supports ATP production and skeletal integrity, while magnesium contributes to over 300 enzymatic reactions and stabilizes DNA and RNA structures. Clinically, hypophosphatemia often manifests with muscle weakness and bone disorders, while hypomagnesemia can cause neuromuscular irritability, cardiac arrhythmias, and electrolyte imbalances.
Causes and Risk Factors
Hypophosphatemia commonly arises from malnutrition, alcoholism, diabetic ketoacidosis, and certain medications like antacids or diuretics reducing phosphate absorption or increasing renal excretion. Hypomagnesemia often results from chronic alcoholism, gastrointestinal losses such as diarrhea or malabsorption, and prolonged use of proton pump inhibitors or diuretics that decrease magnesium levels. Both electrolyte imbalances are frequently observed in critically ill patients, with risks elevated by conditions such as sepsis, burns, or refeeding syndrome.
Pathophysiology: How Each Condition Develops
Hypophosphatemia develops due to impaired phosphate absorption, increased renal phosphate excretion, or intracellular phosphate shifts, often linked to vitamin D deficiency or hyperparathyroidism. Hypomagnesemia results from decreased magnesium intake or absorption, increased renal losses, or shifts due to factors like chronic alcoholism or diuretic use. Both conditions disrupt cellular processes but through distinct mechanisms affecting phosphate and magnesium balance in the body.
Clinical Manifestations and Symptoms
Hypophosphatemia commonly presents with muscle weakness, bone pain, and respiratory failure due to impaired energy metabolism, while hypomagnesemia typically manifests as neuromuscular irritability, including tremors, tetany, and seizures. Cardiovascular symptoms in hypomagnesemia may include arrhythmias and prolonged QT interval, whereas hypophosphatemia can lead to hemolytic anemia and impaired leukocyte function. Both electrolyte imbalances require prompt diagnosis through serum phosphate and magnesium levels to prevent severe complications.
Diagnostic Approaches and Laboratory Findings
Diagnosing hypophosphatemia involves measuring serum phosphate levels, typically below 2.5 mg/dL, alongside assessing urinary phosphate excretion and factors such as vitamin D status and parathyroid hormone levels to identify underlying causes. Hypomagnesemia diagnosis relies on serum magnesium levels, usually under 1.7 mg/dL, with further evaluation including serum calcium, potassium, and renal magnesium wasting tests to differentiate between renal and gastrointestinal losses. Both conditions may require additional tests like electrocardiograms or neuromuscular assessments to evaluate clinical severity and guide treatment.
Treatment and Management Strategies
Treatment of hypophosphatemia involves oral or intravenous phosphate supplementation tailored to the severity of phosphate depletion and underlying causes, with close monitoring of serum phosphate levels to avoid complications like hypocalcemia. Hypomagnesemia management requires magnesium replacement via oral supplements for mild cases and intravenous magnesium sulfate for severe or symptomatic deficiency, alongside correction of contributing factors such as gastrointestinal losses or medications. Both conditions necessitate continuous electrolyte monitoring and addressing etiologies to prevent recurrence and ensure effective recovery.
Complications and Prognosis
Hypophosphatemia can lead to complications such as muscle weakness, respiratory failure, and impaired cardiac function, with severe cases potentially causing rhabdomyolysis and hemolysis. Hypomagnesemia often results in neuromuscular irritability, cardiac arrhythmias, and seizures, with long-term deficiency increasing the risk of osteoporosis and cardiovascular disease. Prognosis for hypophosphatemia improves with prompt phosphate repletion, whereas hypomagnesemia prognosis depends on correcting underlying causes and maintaining magnesium balance to prevent recurrent complications.
Prevention and Monitoring Guidelines
Prevention of hypophosphatemia involves ensuring adequate dietary phosphorus intake and monitoring at-risk populations such as malnourished patients or those on prolonged parenteral nutrition. In contrast, hypomagnesemia prevention emphasizes magnesium-rich diets and careful use of medications like diuretics that promote magnesium loss. Routine monitoring includes serum phosphate and magnesium levels, especially in critically ill patients, with guidelines recommending periodic assessment during refeeding syndrome or chronic gastrointestinal disorders to prevent complications.
Summary and Future Perspectives
Hypophosphatemia, characterized by low serum phosphate levels, primarily affects energy metabolism and bone health, while hypomagnesemia involves reduced magnesium levels critical for enzymatic reactions and neuromuscular function. Emerging research emphasizes the interplay between phosphate and magnesium homeostasis, suggesting integrated diagnostic approaches and targeted therapies. Future perspectives include developing personalized treatment protocols and investigating molecular mechanisms to enhance clinical outcomes in electrolyte imbalance management.
Hypophosphatemia Infographic
 libterm.com
libterm.com