Respiratory alkalosis occurs when excessive breathing reduces carbon dioxide levels in the blood, causing the blood to become too alkaline. Common causes include anxiety, fever, or lung disease, which disrupt the body's acid-base balance. Discover more about the symptoms, causes, and treatment options to better understand how respiratory alkalosis affects your health.
Table of Comparison
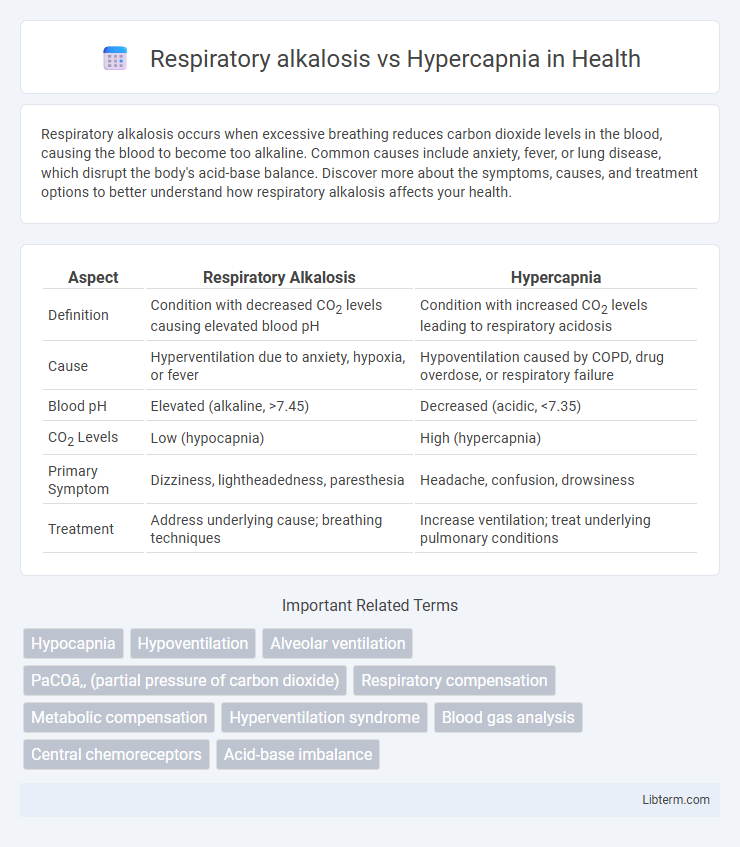
| Aspect | Respiratory Alkalosis | Hypercapnia |
|---|---|---|
| Definition | Condition with decreased CO2 levels causing elevated blood pH | Condition with increased CO2 levels leading to respiratory acidosis |
| Cause | Hyperventilation due to anxiety, hypoxia, or fever | Hypoventilation caused by COPD, drug overdose, or respiratory failure |
| Blood pH | Elevated (alkaline, >7.45) | Decreased (acidic, <7.35) |
| CO2 Levels | Low (hypocapnia) | High (hypercapnia) |
| Primary Symptom | Dizziness, lightheadedness, paresthesia | Headache, confusion, drowsiness |
| Treatment | Address underlying cause; breathing techniques | Increase ventilation; treat underlying pulmonary conditions |
Introduction to Respiratory Alkalosis and Hypercapnia
Respiratory alkalosis is characterized by a decreased partial pressure of carbon dioxide (PaCO2) in arterial blood, resulting from hyperventilation and leading to an elevated blood pH. Hypercapnia, on the other hand, involves an increased PaCO2 due to hypoventilation or impaired gas exchange, causing respiratory acidosis and decreased blood pH. Understanding the pathophysiology and clinical implications of these opposing conditions is crucial for managing respiratory and metabolic imbalances effectively.
Definition and Overview of Respiratory Alkalosis
Respiratory alkalosis is a condition characterized by reduced carbon dioxide (CO2) levels in the blood due to excessive alveolar ventilation, leading to an increase in blood pH above the normal range of 7.35-7.45. It contrasts with hypercapnia, which involves elevated CO2 levels causing respiratory acidosis and decreased blood pH. Respiratory alkalosis commonly results from hyperventilation triggered by anxiety, hypoxia, or pulmonary diseases, disrupting acid-base homeostasis.
Definition and Overview of Hypercapnia
Hypercapnia is a condition characterized by an elevated level of carbon dioxide (CO2) in the blood, typically resulting from hypoventilation or impaired gas exchange in the lungs. Respiratory alkalosis, in contrast, occurs when excess CO2 is exhaled due to hyperventilation, leading to a decrease in blood CO2 levels and an increase in blood pH. Understanding the pathophysiological mechanisms that differentiate hypercapnia and respiratory alkalosis is critical for accurate diagnosis and effective treatment of respiratory disorders.
Key Differences Between Respiratory Alkalosis and Hypercapnia
Respiratory alkalosis is characterized by decreased arterial carbon dioxide (PaCO2) leading to elevated blood pH due to hyperventilation, while hypercapnia involves increased PaCO2 caused by hypoventilation or impaired gas exchange resulting in respiratory acidosis. The primary clinical distinction lies in the direction of PaCO2 levels; respiratory alkalosis exhibits low PaCO2 (<35 mmHg), whereas hypercapnia shows high PaCO2 (>45 mmHg). Symptoms of respiratory alkalosis often include lightheadedness and paresthesia, contrasting with hypercapnia symptoms such as headache, confusion, and somnolence related to increased CO2 retention.
Pathophysiology: Mechanisms Behind Each Condition
Respiratory alkalosis results from excessive alveolar ventilation causing a decrease in arterial carbon dioxide (PaCO2) levels, leading to increased blood pH due to reduced carbonic acid concentration. Hypercapnia, characterized by elevated PaCO2, arises from hypoventilation or impaired gas exchange, causing respiratory acidosis through accumulation of carbonic acid and lowered blood pH. The primary pathophysiological difference lies in the ventilatory drive and gas exchange efficiency: respiratory alkalosis involves hyperventilation reducing CO2, while hypercapnia stems from inadequate ventilation or diffusion defects causing CO2 retention.
Causes and Risk Factors
Respiratory alkalosis is primarily caused by hyperventilation due to anxiety, fever, or hypoxemia, leading to decreased carbon dioxide levels in the blood. Hypercapnia, on the other hand, results from hypoventilation or impaired gas exchange seen in chronic obstructive pulmonary disease (COPD), neuromuscular disorders, or respiratory failure, causing elevated carbon dioxide retention. Risk factors for respiratory alkalosis include acute stress and pulmonary embolism, while hypercapnia risk factors encompass obesity hypoventilation syndrome and severe asthma exacerbations.
Clinical Signs and Symptoms
Respiratory alkalosis typically presents with clinical signs such as lightheadedness, confusion, paresthesia, and muscle twitching due to decreased carbon dioxide levels and resultant cerebral vasoconstriction. In contrast, hypercapnia is characterized by symptoms including headache, flushed skin, drowsiness, and dyspnea, reflecting elevated carbon dioxide levels and respiratory acidosis. Both conditions affect acid-base balance but manifest distinct clinical features related to their underlying respiratory pathophysiology.
Diagnostic Approaches and Laboratory Findings
Respiratory alkalosis is characterized by decreased arterial carbon dioxide tension (PaCO2) below 35 mmHg, often diagnosed through arterial blood gas (ABG) analysis showing elevated blood pH and low PaCO2, with potential compensatory decrease in bicarbonate. In contrast, hypercapnia is identified by elevated PaCO2 above 45 mmHg on ABG, frequently accompanied by respiratory acidosis with decreased pH and elevated bicarbonate in chronic cases. Diagnostic approaches integrate clinical assessment with laboratory findings, including ABG and serum electrolytes, to distinguish between primary respiratory alkalosis and hypercapnic respiratory failure.
Management and Treatment Strategies
Management of respiratory alkalosis involves addressing the underlying cause such as anxiety, pain, or hypoxemia, often with controlled breathing techniques and correction of oxygen levels. In contrast, hypercapnia treatment focuses on improving alveolar ventilation through non-invasive ventilation like CPAP or BiPAP and treating respiratory failure causes, including obstructive lung diseases. Monitoring arterial blood gases guides therapy adjustments to normalize pH and carbon dioxide levels efficiently.
Prognosis and Potential Complications
Respiratory alkalosis typically has a favorable prognosis when underlying causes such as hyperventilation or anxiety are promptly treated, but persistent alkalosis may lead to complications like neuromuscular irritability or cardiac arrhythmias. Hypercapnia, characterized by elevated arterial CO2 levels, carries a more guarded prognosis due to risks of respiratory failure, altered mental status, and potential progression to respiratory acidosis if untreated. Both conditions require targeted interventions to prevent severe sequelae, with hypercapnia posing a higher risk of morbidity and mortality due to impaired gas exchange and tissue hypoxia.
Respiratory alkalosis Infographic
 libterm.com
libterm.com