Hyperparathyroidism occurs when the parathyroid glands produce excessive parathyroid hormone, leading to elevated calcium levels in the blood which can cause bone pain, kidney stones, and fatigue. Early diagnosis and treatment are crucial to prevent complications such as osteoporosis and cardiovascular issues. Discover effective management strategies and symptoms to watch for in the rest of this article.
Table of Comparison
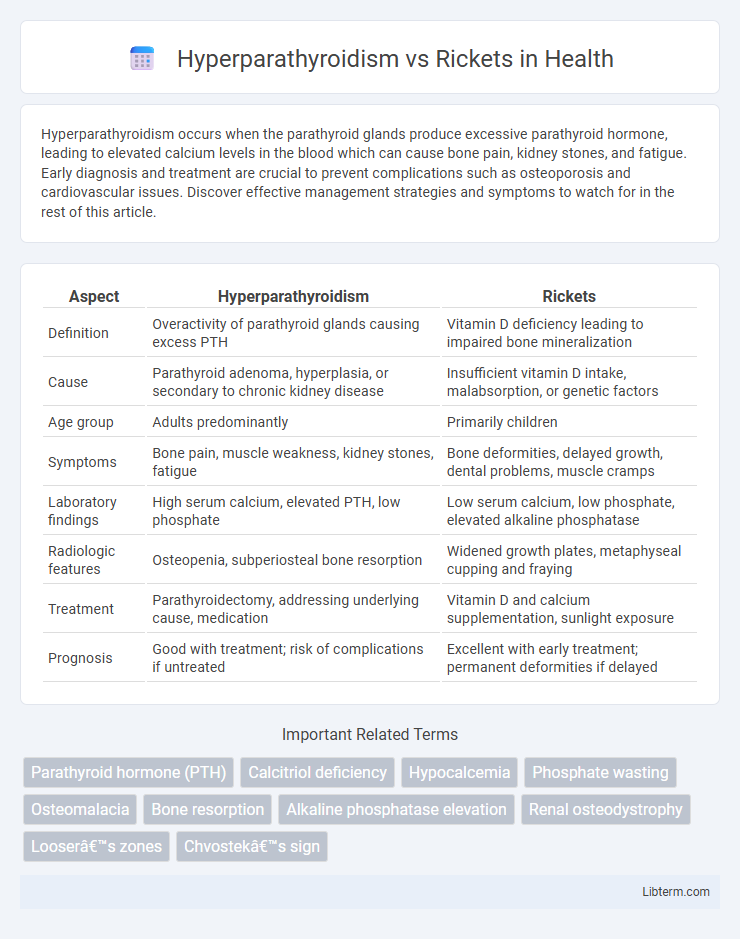
| Aspect | Hyperparathyroidism | Rickets |
|---|---|---|
| Definition | Overactivity of parathyroid glands causing excess PTH | Vitamin D deficiency leading to impaired bone mineralization |
| Cause | Parathyroid adenoma, hyperplasia, or secondary to chronic kidney disease | Insufficient vitamin D intake, malabsorption, or genetic factors |
| Age group | Adults predominantly | Primarily children |
| Symptoms | Bone pain, muscle weakness, kidney stones, fatigue | Bone deformities, delayed growth, dental problems, muscle cramps |
| Laboratory findings | High serum calcium, elevated PTH, low phosphate | Low serum calcium, low phosphate, elevated alkaline phosphatase |
| Radiologic features | Osteopenia, subperiosteal bone resorption | Widened growth plates, metaphyseal cupping and fraying |
| Treatment | Parathyroidectomy, addressing underlying cause, medication | Vitamin D and calcium supplementation, sunlight exposure |
| Prognosis | Good with treatment; risk of complications if untreated | Excellent with early treatment; permanent deformities if delayed |
Introduction to Hyperparathyroidism and Rickets
Hyperparathyroidism is a condition characterized by excessive secretion of parathyroid hormone, leading to elevated calcium levels and disrupted bone metabolism. Rickets is a pediatric disorder caused by vitamin D deficiency, resulting in impaired bone mineralization and skeletal deformities. Both disorders affect bone health but differ in hormonal and nutritional etiology.
Overview of Calcium and Phosphate Homeostasis
Calcium and phosphate homeostasis is tightly regulated by parathyroid hormone (PTH), vitamin D, and calcitonin to maintain bone mineralization and cellular functions. Hyperparathyroidism causes excessive PTH secretion, leading to increased calcium resorption from bones, decreased phosphate reabsorption in kidneys, and elevated serum calcium with low phosphate levels. In contrast, rickets results from vitamin D deficiency or phosphate metabolism disorders, causing impaired calcium and phosphate absorption, leading to low serum calcium and phosphate, defective bone mineralization, and skeletal deformities.
Etiology: Causes of Hyperparathyroidism
Hyperparathyroidism is primarily caused by parathyroid gland adenomas, hyperplasia, or, rarely, parathyroid carcinoma, leading to excessive secretion of parathyroid hormone (PTH). Secondary hyperparathyroidism results from chronic kidney disease or vitamin D deficiency that causes hypocalcemia and compensatory PTH overproduction. In contrast, rickets arises from deficiencies in vitamin D, calcium, or phosphate, causing impaired bone mineralization rather than hormone hypersecretion.
Etiology: Causes of Rickets
Rickets primarily results from vitamin D deficiency, leading to impaired calcium and phosphate metabolism essential for bone mineralization. Nutritional insufficiency, limited sunlight exposure, and malabsorption disorders contribute significantly to its etiology. Unlike hyperparathyroidism, which involves excessive parathyroid hormone secretion often due to gland hyperplasia or adenoma, rickets is fundamentally a disorder of bone development caused by inadequate mineral availability.
Clinical Manifestations: Signs and Symptoms
Hyperparathyroidism presents with hypercalcemia, muscle weakness, bone pain, kidney stones, and neuropsychiatric symptoms such as fatigue and depression. Rickets is characterized by bone deformities including bowed legs, delayed growth, dental problems, and skeletal tenderness due to defective mineralization caused by vitamin D deficiency. Both conditions involve bone abnormalities but differ in their metabolic causes and specific clinical features.
Pathophysiological Differences
Hyperparathyroidism involves excessive secretion of parathyroid hormone (PTH), leading to increased bone resorption, elevated serum calcium, and decreased phosphate levels as PTH mobilizes calcium from bones and reduces renal phosphate reabsorption. Rickets results from vitamin D deficiency or phosphate metabolism disorders that impair bone mineralization, causing hypocalcemia, hypophosphatemia, and defective growth plate calcification. The primary pathophysiological difference lies in hyperparathyroidism causing calcium excess and bone demineralization through PTH overactivity, whereas rickets is characterized by inadequate bone mineralization due to vitamin D or phosphate deficiency.
Diagnostic Criteria and Laboratory Findings
Hyperparathyroidism is diagnosed through elevated serum calcium levels, low to normal phosphate, and markedly increased parathyroid hormone (PTH) levels, along with imaging such as sestamibi scans or neck ultrasound for adenoma localization. Rickets is characterized by low serum calcium, low phosphate, elevated alkaline phosphatase, and increased parathyroid hormone secondary to vitamin D deficiency or phosphate metabolism disorders, confirmed by radiographic evidence of metaphyseal cupping and fraying in growing bones. Laboratory findings distinguish hyperparathyroidism by hypercalcemia and high PTH, whereas rickets shows hypocalcemia or normocalcemia with secondary hyperparathyroidism and vitamin D insufficiency.
Imaging Features in Hyperparathyroidism and Rickets
Imaging features of hyperparathyroidism typically include subperiosteal bone resorption, especially along the radial aspects of the middle phalanges, salt-and-pepper skull appearance, and brown tumors visible on X-rays or MRI. Rickets presents with metaphyseal cupping, fraying, and widening in long bones, along with generalized osteopenia and bowing of the legs on radiographs. Unlike rickets, hyperparathyroidism shows more focal bone resorption and skeletal erosions linked to excessive parathyroid hormone levels affecting calcium metabolism.
Treatment Modalities: Comparison and Strategies
Treatment modalities for hyperparathyroidism primarily involve surgical intervention, such as parathyroidectomy, to remove overactive glands, alongside calcium and vitamin D supplementation to manage bone density. In contrast, rickets treatment centers on replenishing deficient vitamin D, calcium, and phosphate through dietary modifications and supplementation to promote proper bone mineralization. While hyperparathyroidism addresses hormone regulation and glandular function, rickets management focuses on correcting nutritional deficiencies to prevent skeletal deformities.
Prognosis and Long-term Complications
Hyperparathyroidism prognosis varies with early diagnosis and treatment, typically resulting in normalization of calcium levels and reduced risk of bone loss, kidney stones, and cardiovascular complications. Rickets, primarily caused by vitamin D deficiency, has a favorable prognosis if treated promptly with supplementation, but delayed intervention may lead to irreversible bone deformities and growth retardation. Long-term complications of untreated hyperparathyroidism include osteoporosis, nephrocalcinosis, and neuropsychiatric disorders, whereas untreated rickets can cause permanent skeletal deformities and dental problems.
Hyperparathyroidism Infographic
 libterm.com
libterm.com