Mucolytic agents work by breaking down mucus, making it thinner and easier to clear from the respiratory tract, which helps improve breathing and reduce congestion. These medications are commonly used to treat conditions such as chronic bronchitis, cystic fibrosis, and asthma. Discover how mucolytics can benefit your respiratory health by reading the full article.
Table of Comparison
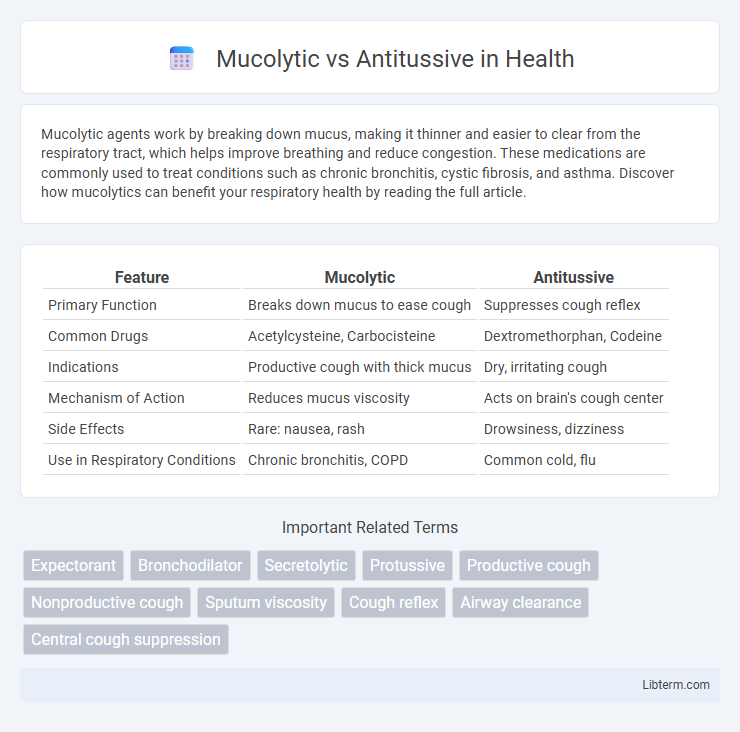
| Feature | Mucolytic | Antitussive |
|---|---|---|
| Primary Function | Breaks down mucus to ease cough | Suppresses cough reflex |
| Common Drugs | Acetylcysteine, Carbocisteine | Dextromethorphan, Codeine |
| Indications | Productive cough with thick mucus | Dry, irritating cough |
| Mechanism of Action | Reduces mucus viscosity | Acts on brain's cough center |
| Side Effects | Rare: nausea, rash | Drowsiness, dizziness |
| Use in Respiratory Conditions | Chronic bronchitis, COPD | Common cold, flu |
Introduction to Cough Management
Mucolytics target mucus viscosity by breaking down its structure to facilitate easier expectoration in respiratory conditions with thick, sticky secretions. Antitussives suppress the cough reflex, providing relief in cases where cough is dry and non-productive, preventing irritation and improving patient comfort. Effective cough management often requires selecting the appropriate therapeutic approach based on cough type to optimize treatment outcomes.
Understanding Mucolytics: Definition and Mechanism
Mucolytics are pharmacological agents designed to break down mucus structure by cleaving the mucoprotein bonds, resulting in decreased viscosity and easier expectoration. They enhance mucus clearance from the respiratory tract by reducing mucus thickness, thereby facilitating respiratory function. Unlike antitussives, which suppress cough reflex, mucolytics specifically target mucus properties to improve airway patency and reduce congestion.
What Are Antitussives? Mechanisms and Types
Antitussives are medications designed to suppress or reduce coughing by acting on the cough center in the brain or the nerves involved in the cough reflex. Common mechanisms include central suppression via opioids like codeine and dextromethorphan, or peripheral action through anesthetics such as benzonatate. Types of antitussives include opioid and non-opioid agents, with non-opioids preferred for their lower risk of dependency and side effects.
Key Differences: Mucolytic vs Antitussive
Mucolytics work by breaking down mucus to reduce its viscosity and facilitate easier expectoration, whereas antitussives suppress the cough reflex to decrease coughing frequency or intensity. Mucolytics are typically used in conditions with thick, productive coughs, such as chronic bronchitis or cystic fibrosis, while antitussives are preferred for dry, non-productive coughs often seen in viral upper respiratory infections. Understanding these mechanisms helps tailor treatments for respiratory conditions by either enhancing mucus clearance or alleviating cough symptoms.
Indications for Mucolytic Use
Mucolytics are primarily indicated for conditions characterized by excessive or thick mucus production, such as chronic bronchitis, cystic fibrosis, and chronic obstructive pulmonary disease (COPD). These agents work by breaking down the mucus structure to facilitate easier expectoration and improve airway clearance. Their use is essential in managing respiratory infections and disorders where mucus viscosity impedes normal respiratory function.
When to Choose an Antitussive
Antitussives are best chosen when the cough is dry, persistent, and nonproductive, as they suppress the cough reflex to provide relief and improve sleep quality. In contrast, mucolytics are preferred for productive coughs where mucus needs to be loosened and expelled from the respiratory tract. Selecting an antitussive is crucial in conditions like nocturnal cough or when coughing causes significant discomfort or impairs daily functioning without the presence of mucus accumulation.
Efficacy and Safety: Clinical Evidence
Mucolytics demonstrate efficacy by breaking down mucus to improve airway clearance, as evidenced in clinical trials showing reduced sputum viscosity and enhanced expectoration in chronic bronchitis patients. Antitussives act by suppressing the cough reflex, with studies highlighting their use in managing dry, non-productive coughs, though concerns about potential respiratory depression warrant cautious use. Safety profiles indicate mucolytics are generally well-tolerated with minimal adverse effects, while antitussives require careful dosing to avoid side effects such as sedation or respiratory compromise, especially in vulnerable populations.
Side Effects and Contraindications
Mucolytics frequently cause gastrointestinal disturbances such as nausea, vomiting, and diarrhea, and are contraindicated in patients with peptic ulcers or asthma due to potential airway irritation. Antitussives may induce drowsiness, dizziness, and constipation, and are contraindicated in children under certain ages, patients with chronic respiratory conditions like asthma or COPD, and those on monoamine oxidase inhibitors (MAOIs) because of risk of severe side effects. Careful assessment of patient history is essential to avoid adverse reactions and contraindications related to both drug classes.
Special Considerations: Age, Pregnancy, and Comorbidities
Mucolytic agents, such as acetylcysteine, are generally preferred in pediatric and elderly patients due to their ability to thin mucus without suppressing the cough reflex, which is crucial for airway clearance. Antitussives like dextromethorphan require caution during pregnancy and in patients with respiratory comorbidities such as asthma or COPD, as cough suppression may exacerbate mucus retention and increase the risk of infections. Special considerations include dosage adjustments and careful assessment of potential drug interactions in pregnant women and those with hepatic or renal impairment.
Conclusion: Selecting the Right Cough Treatment
Mucolytics effectively reduce mucus viscosity, facilitating easier expectoration in productive coughs, while antitussives suppress the cough reflex, providing relief for dry, non-productive coughs. Selecting the right cough treatment depends on the underlying cause and cough type, with mucolytics preferred for bronchitis or chronic respiratory conditions and antitussives suited for temporary relief of irritating, dry coughs. Proper diagnosis and symptom evaluation are crucial to optimize therapeutic outcomes and avoid inappropriate medication use.
Mucolytic Infographic
 libterm.com
libterm.com