Leukoplakia and lichen planus are common oral mucosal conditions characterized by white patches that can sometimes indicate underlying health issues. Early detection and accurate diagnosis are essential to prevent potential progression into more serious conditions like oral cancer. Discover how to recognize symptoms and explore effective treatment options in the rest of this article.
Table of Comparison
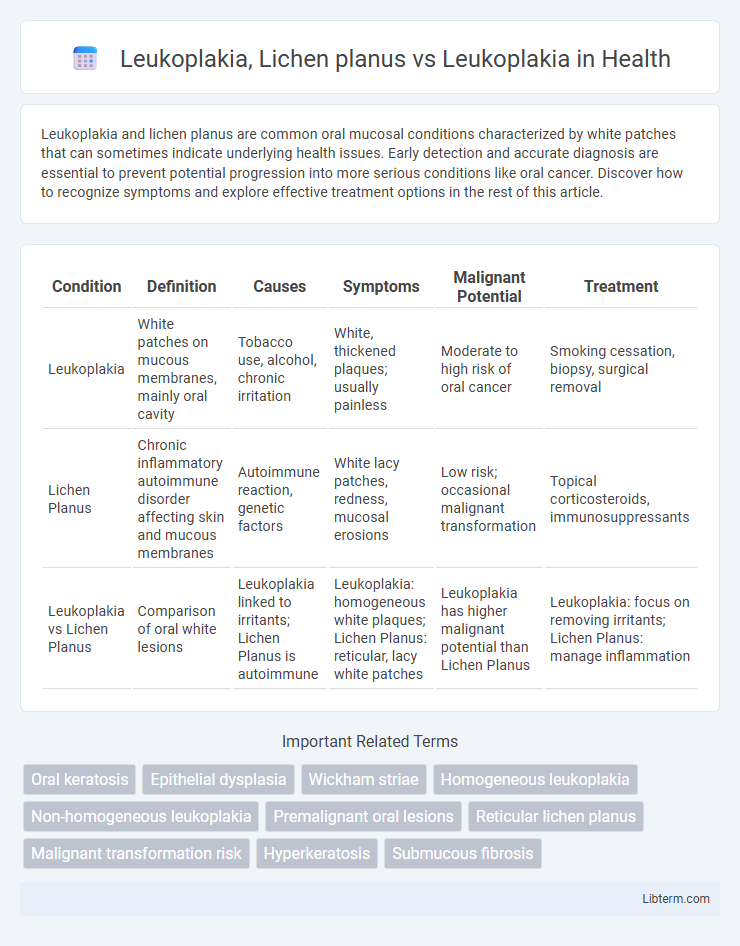
| Condition | Definition | Causes | Symptoms | Malignant Potential | Treatment |
|---|---|---|---|---|---|
| Leukoplakia | White patches on mucous membranes, mainly oral cavity | Tobacco use, alcohol, chronic irritation | White, thickened plaques; usually painless | Moderate to high risk of oral cancer | Smoking cessation, biopsy, surgical removal |
| Lichen Planus | Chronic inflammatory autoimmune disorder affecting skin and mucous membranes | Autoimmune reaction, genetic factors | White lacy patches, redness, mucosal erosions | Low risk; occasional malignant transformation | Topical corticosteroids, immunosuppressants |
| Leukoplakia vs Lichen Planus | Comparison of oral white lesions | Leukoplakia linked to irritants; Lichen Planus is autoimmune | Leukoplakia: homogeneous white plaques; Lichen Planus: reticular, lacy white patches | Leukoplakia has higher malignant potential than Lichen Planus | Leukoplakia: focus on removing irritants; Lichen Planus: manage inflammation |
Introduction to Oral Leukoplakia
Oral Leukoplakia is a white patch or plaque that cannot be rubbed off and cannot be characterized clinically or pathologically as any other condition, often associated with tobacco use and chronic irritation. Lichen planus, a chronic inflammatory condition affecting the mucous membranes, can present with white, lacy patterns but differs from leukoplakia in etiology and microscopic features. Understanding the distinct clinical presentations and histopathological characteristics of Oral Leukoplakia versus Lichen Planus is crucial for accurate diagnosis and effective management.
Understanding Oral Lichen Planus
Oral Lichen Planus is a chronic inflammatory condition characterized by white, lace-like patches on the mucous membranes inside the mouth, differing from Leukoplakia, which presents as thickened, white plaques that cannot be scraped off. Unlike Leukoplakia, a potential precancerous lesion, Oral Lichen Planus is primarily autoimmune in nature and often causes discomfort or pain. Diagnosis relies on clinical examination and biopsy to distinguish between these conditions due to their overlapping presentations but differing management and malignancy risks.
Epidemiology and Risk Factors
Leukoplakia primarily affects middle-aged to older adults with a higher prevalence among tobacco users and individuals exposed to alcohol, showing a global incidence of approximately 1-2%, with men being more commonly affected. Oral Lichen Planus is a chronic inflammatory condition predominantly seen in middle-aged women, with a prevalence ranging from 0.5% to 2%, and is not strongly linked to tobacco or alcohol use. Both conditions share risk factors such as chronic irritation and immune dysregulation but differ significantly in demographic distribution and associations with carcinogenic exposures.
Clinical Presentation: Leukoplakia vs. Lichen Planus
Leukoplakia presents as white, non-removable plaques on the oral mucosa, often with a rough or verrucous surface, predominantly affecting smokers and individuals with tobacco use. In contrast, oral lichen planus typically manifests as bilateral, lace-like reticular white lines (Wickham's striae) accompanied by erythematous and erosive lesions, reflecting its autoimmune etiology. While leukoplakia is a potentially premalignant lesion requiring biopsy for dysplasia evaluation, lichen planus exhibits chronic inflammation with variable symptoms such as burning sensation or asymptomatic white patches.
Histopathological Differences
Leukoplakia histopathology reveals hyperkeratosis, acanthosis, and variable degrees of epithelial dysplasia with no significant inflammatory infiltrate, while lichen planus displays a band-like lymphocytic infiltrate at the dermoepidermal junction, basal cell degeneration, and saw-tooth rete ridges. Leukoplakia presents with epithelial thickening and keratin layer abnormalities, frequently associated with premalignant changes. In contrast, lichen planus shows prominent interface dermatitis and Civatte bodies, reflecting an immune-mediated pathogenesis.
Diagnosis and Differential Diagnosis
Leukoplakia diagnosis involves clinical examination and histopathological analysis to identify hyperkeratotic plaques with potential dysplasia, while lichen planus is characterized by Wickham striae and a band-like lymphocytic infiltrate on biopsy. Differential diagnosis requires distinguishing leukoplakia from lichen planus by evaluating lesion morphology, distribution, and histological features such as basal cell degeneration in lichen planus versus epithelial dysplasia in leukoplakia. Immunofluorescence studies and exclusion of other white lesions like candidiasis and lupus erythematosus further aid in accurate differentiation.
Malignant Transformation Potential
Leukoplakia exhibits a higher malignant transformation potential, with rates ranging from 1% to 20%, particularly in non-homogeneous and verrucous types, making it a significant precancerous lesion. Oral lichen planus shows a comparatively lower risk of malignant conversion, estimated between 0.5% and 2%, primarily linked to the erosive and atrophic variants. Close clinical monitoring and biopsy of suspicious leukoplakia lesions are critical for early detection and prevention of oral squamous cell carcinoma.
Current Treatment Modalities
Current treatment modalities for leukoplakia primarily include surgical excision, laser therapy, and cryotherapy, with regular monitoring for malignant transformation due to its potential precancerous nature. Lichen planus management emphasizes corticosteroids, both topical and systemic, to reduce inflammation and immune response, alongside immunomodulators like tacrolimus for resistant cases. Both conditions require ongoing clinical evaluation to detect dysplastic changes early and tailor interventions accordingly.
Prognosis and Recurrence Rates
Leukoplakia presents a variable prognosis with a malignant transformation rate ranging from 1% to 20%, depending on histopathological features such as dysplasia severity, while recurrence rates after treatment can reach up to 30%. Lichen planus, particularly the erosive type, demonstrates a lower but notable risk of malignant transformation estimated between 0.4% and 3.5%, with chronic inflammation contributing to persistent recurrence and symptom exacerbation. Careful long-term monitoring and biopsy of suspicious lesions are critical for both conditions due to their potential for malignancy and high recurrence probability.
Prevention and Patient Education
Preventing leukoplakia and lichen planus involves minimizing risk factors such as tobacco use, alcohol consumption, and chronic irritation from dental appliances. Patient education emphasizes regular oral hygiene, routine dental check-ups, and prompt reporting of persistent white patches or lesions to enable early diagnosis and management. Understanding these preventive measures reduces the risk of malignant transformation, particularly in leukoplakia, which carries a higher potential for oral cancer development.
Leukoplakia, Lichen planus Infographic
 libterm.com
libterm.com