Hyperpnea is characterized by an increased depth and rate of breathing, often occurring in response to heightened physical activity or metabolic demands. Unlike hyperventilation, which involves excessive ventilation leading to a decrease in carbon dioxide levels, hyperpnea matches the body's need for oxygen without disrupting blood gas balance. Explore the full article to understand the causes, symptoms, and management of hyperpnea and how it affects your respiratory health.
Table of Comparison
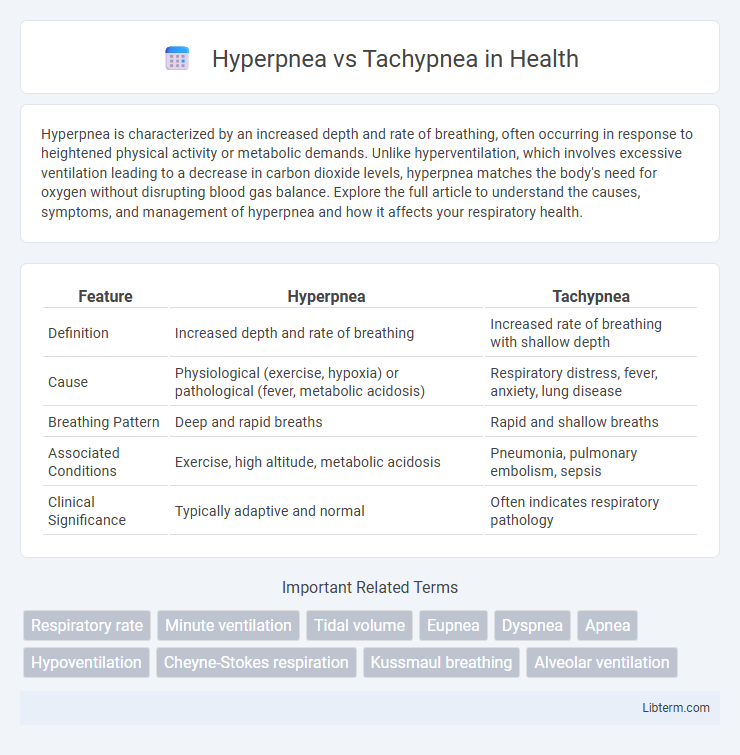
| Feature | Hyperpnea | Tachypnea |
|---|---|---|
| Definition | Increased depth and rate of breathing | Increased rate of breathing with shallow depth |
| Cause | Physiological (exercise, hypoxia) or pathological (fever, metabolic acidosis) | Respiratory distress, fever, anxiety, lung disease |
| Breathing Pattern | Deep and rapid breaths | Rapid and shallow breaths |
| Associated Conditions | Exercise, high altitude, metabolic acidosis | Pneumonia, pulmonary embolism, sepsis |
| Clinical Significance | Typically adaptive and normal | Often indicates respiratory pathology |
Introduction to Hyperpnea and Tachypnea
Hyperpnea and tachypnea are respiratory conditions characterized by variations in breathing patterns. Hyperpnea involves an increased depth and rate of breathing, often as a physiological response to increased oxygen demand, such as during exercise or metabolic acidosis. Tachypnea is defined by abnormally rapid and shallow breathing, commonly associated with respiratory distress, fever, or pulmonary disorders.
Defining Hyperpnea: Meaning and Characteristics
Hyperpnea refers to an increased depth and rate of breathing, often seen during exercise or metabolic demand, characterized by deep, rapid breaths that enhance oxygen intake and carbon dioxide elimination. Unlike tachypnea, which involves only rapid shallow breaths, hyperpnea maintains or increases tidal volume to match heightened physiological needs. This respiratory pattern is typically normal in response to physical activity, stress, or certain medical conditions such as metabolic acidosis.
Understanding Tachypnea: Key Features
Tachypnea is characterized by an abnormally rapid breathing rate, generally exceeding 20 breaths per minute in adults, often signaling underlying conditions such as fever, anxiety, or respiratory distress. It differs from hyperpnea, which involves increased depth and rate of breathing linked to metabolic demand rather than pathology. Recognizing tachypnea's key features--rapid, shallow breaths without adequate ventilation--is crucial for early diagnosis and treatment of respiratory illnesses.
Physiological Causes of Hyperpnea
Hyperpnea is characterized by an increased depth and rate of breathing, often triggered by physiological demands such as exercise, high altitude, or metabolic acidosis, leading to enhanced alveolar ventilation. In contrast, tachypnea involves rapid, shallow breathing primarily caused by conditions that increase respiratory rate without significantly changing tidal volume, such as fever, pain, or lung injury. The physiological causes of hyperpnea include increased carbon dioxide production and oxygen consumption during physical activity, stimulating the respiratory centers in the brainstem to elevate ventilation.
Common Triggers of Tachypnea
Tachypnea is commonly triggered by conditions causing hypoxia, such as pneumonia, pulmonary embolism, or acute asthma exacerbations, resulting in rapid, shallow breathing to increase oxygen intake. Hyperpnea, characterized by increased depth and rate of breathing, often arises during exercise or metabolic acidosis as the body demands more oxygen or needs to expel excess carbon dioxide. Recognizing tachypnea's association with respiratory distress and systemic illnesses is crucial for prompt diagnosis and treatment.
Differences in Respiratory Patterns
Hyperpnea is characterized by an increased depth and rate of breathing, typically in response to metabolic demands like exercise or acidosis, allowing more efficient oxygen intake and carbon dioxide elimination. Tachypnea involves rapid, shallow breathing that primarily increases respiratory rate without significant increase in tidal volume, often seen in conditions such as fever, anxiety, or respiratory distress. The key distinction lies in hyperpnea's augmentation of tidal volume and rate versus tachypnea's elevation of rate alone, impacting overall ventilation efficiency and gas exchange.
Clinical Implications and Diagnosis
Hyperpnea, characterized by an increased depth and rate of breathing, often indicates metabolic acidosis or increased oxygen demand in conditions such as sepsis or exercise, whereas tachypnea, defined as an elevated respiratory rate with shallow breaths, commonly signals respiratory distress or pulmonary pathologies like pneumonia or pulmonary embolism. Clinically, distinguishing between hyperpnea and tachypnea guides diagnosis, with hyperpnea linked to systemic causes assessed through arterial blood gases and lactate levels, while tachypnea prompts evaluation of lung function, chest imaging, and oxygen saturation to detect underlying respiratory compromise. Accurate recognition drives appropriate treatment strategies, optimizing patient outcomes by targeting the specific pathophysiological mechanism responsible for the altered breathing pattern.
When to Seek Medical Attention
Seek medical attention for hyperpnea if rapid, deep breathing is accompanied by chest pain, dizziness, or lasting more than a few minutes, indicating possible respiratory or metabolic issues. Tachypnea requires urgent evaluation when breathing rate exceeds 20 breaths per minute at rest and is associated with shortness of breath, cyanosis, or altered mental status. Prompt medical assessment is critical to address underlying causes such as infections, heart failure, or pulmonary embolism in both conditions.
Management and Treatment Approaches
Management of hyperpnea focuses on addressing underlying causes such as metabolic acidosis or respiratory compensation by ensuring adequate oxygenation and correcting acid-base imbalances through interventions like bicarbonate therapy. Tachypnea treatment emphasizes identifying and resolving the root cause, including infections, pulmonary embolism, or heart failure, often requiring antibiotics, anticoagulants, or diuretics as appropriate. Both conditions benefit from continuous monitoring of respiratory rate, oxygen saturation, and arterial blood gases to guide therapy and ensure resolution of abnormal breathing patterns.
Summary: Hyperpnea vs. Tachypnea Comparison
Hyperpnea refers to increased depth and rate of breathing often linked to physiological demand such as exercise, while tachypnea describes abnormally rapid breathing typically associated with respiratory distress or pathology. Hyperpnea maintains or enhances alveolar ventilation effectively, ensuring adequate oxygen and carbon dioxide exchange, whereas tachypnea may lead to inefficient ventilation and respiratory alkalosis. Differentiating these conditions is critical for clinical assessment, as hyperpnea is usually non-pathological, whereas tachypnea often signals underlying respiratory or systemic illness.
Hyperpnea Infographic
 libterm.com
libterm.com