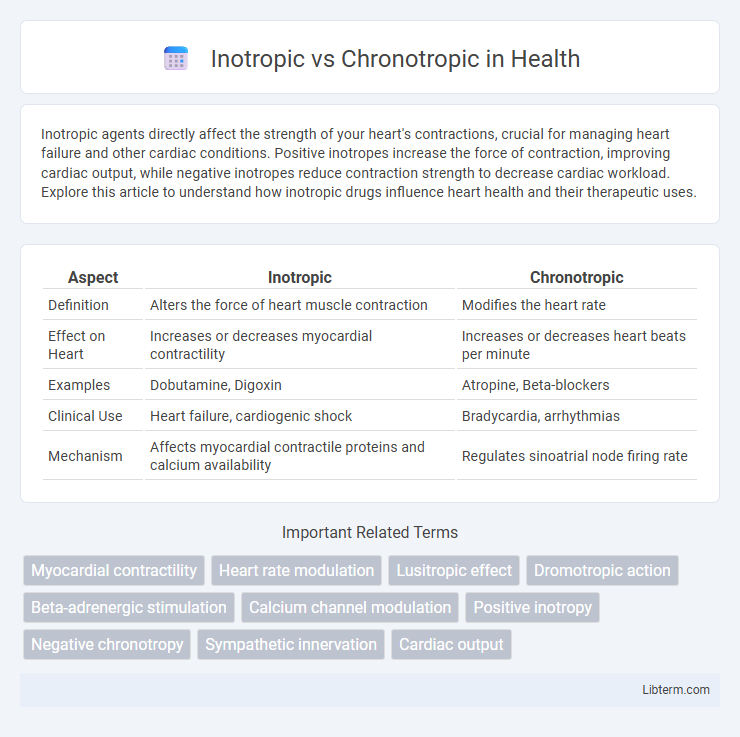
Inotropic agents directly affect the strength of your heart's contractions, crucial for managing heart failure and other cardiac conditions. Positive inotropes increase the force of contraction, improving cardiac output, while negative inotropes reduce contraction strength to decrease cardiac workload. Explore this article to understand how inotropic drugs influence heart health and their therapeutic uses.
Table of Comparison
| Aspect | Inotropic | Chronotropic |
|---|---|---|
| Definition | Alters the force of heart muscle contraction | Modifies the heart rate |
| Effect on Heart | Increases or decreases myocardial contractility | Increases or decreases heart beats per minute |
| Examples | Dobutamine, Digoxin | Atropine, Beta-blockers |
| Clinical Use | Heart failure, cardiogenic shock | Bradycardia, arrhythmias |
| Mechanism | Affects myocardial contractile proteins and calcium availability | Regulates sinoatrial node firing rate |
Introduction to Inotropic and Chronotropic Effects
Inotropic effects refer to changes in the strength or force of cardiac muscle contractions, directly influencing stroke volume and cardiac output. Chronotropic effects impact the heart rate by altering the frequency of electrical impulses generated by the sinoatrial node. Both inotropic and chronotropic mechanisms play critical roles in cardiovascular function and are targeted in various treatments for heart conditions.
Defining Inotropic Actions
Inotropic actions refer to the effects on the strength or force of cardiac muscle contraction, primarily influenced by changes in intracellular calcium levels. Positive inotropic agents increase myocardial contractility, improving stroke volume and cardiac output, while negative inotropic agents reduce contractile force. Understanding inotropic mechanisms is critical in managing heart failure and other cardiac conditions where modulation of contractile strength is necessary.
Understanding Chronotropic Responses
Chronotropic responses refer to changes in heart rate influenced by the autonomic nervous system, primarily through alterations in the sinoatrial node's pacing activity. These responses are critical in regulating cardiac output during physical activity or stress by increasing or decreasing the heart rate. Understanding chronotropic effects aids in managing conditions like arrhythmias, heart failure, and the impacts of medications such as beta-blockers on cardiac function.
Key Differences: Inotropic vs Chronotropic
Inotropic effects refer to the force or strength of heart muscle contractions, directly influencing cardiac output by altering myocardial contractility. Chronotropic effects impact the heart rate by affecting the sinoatrial node, thereby modifying the frequency of cardiac cycles per minute. Understanding the distinction between inotropic modulation (contractile force) and chronotropic modulation (heart rate) is essential in cardiovascular pharmacology and clinical treatments for heart conditions.
Mechanisms of Inotropic Effects
Inotropic effects primarily alter the force of myocardial contraction by modulating calcium ion availability within cardiac muscle cells, which directly influences contractility. Positive inotropic agents increase intracellular calcium concentration through mechanisms such as enhanced calcium influx via L-type calcium channels or increased release from the sarcoplasmic reticulum, thereby strengthening cardiac output. Negative inotropic effects reduce calcium availability or impair calcium sensitivity in cardiac myofilaments, resulting in decreased contractile force without necessarily affecting heart rate.
Mechanisms of Chronotropic Regulation
Chronotropic regulation primarily involves the modulation of heart rate through autonomic nervous system inputs, where sympathetic stimulation increases heart rate by enhancing the pacemaker activity of the sinoatrial node via beta-adrenergic receptor activation and increased cAMP production. Parasympathetic influence decreases heart rate through acetylcholine release, which activates muscarinic M2 receptors, leading to the opening of potassium channels and hyperpolarization of pacemaker cells. These signaling pathways adjust the timing of action potentials in the sinoatrial node, thereby controlling the frequency of cardiac contractions.
Clinical Significance in Cardiology
Inotropic effects directly influence myocardial contractility, crucial for managing heart failure by improving cardiac output and tissue perfusion. Chronotropic effects regulate heart rate, essential in treating arrhythmias and optimizing cardiac workload. Precise modulation of inotropic and chronotropic responses is vital in cardiology to enhance patient outcomes in conditions such as heart failure, atrial fibrillation, and ischemic heart disease.
Common Drugs Influencing Inotropy and Chronotropy
Common drugs influencing inotropy include digoxin, which increases myocardial contractility by inhibiting the sodium-potassium ATPase pump, and dobutamine, a beta-1 adrenergic agonist that enhances cardiac output through positive inotropic effects. Chronotropic drugs primarily affect heart rate and include beta blockers like metoprolol, which decrease heart rate by blocking beta-1 receptors, and atropine, an anticholinergic that increases heart rate by inhibiting parasympathetic stimulation. Understanding the pharmacodynamics of inotropic and chronotropic agents is crucial for managing heart failure, arrhythmias, and other cardiovascular conditions.
Diagnostic Methods for Evaluating Cardiac Function
Inotropic and chronotropic effects are crucial parameters in assessing cardiac function, where inotropic relates to myocardial contractility and chronotropic refers to heart rate regulation. Diagnostic methods such as echocardiography with Doppler imaging, cardiac MRI, and invasive hemodynamic monitoring provide detailed evaluation of inotropic function by measuring ventricular wall motion and ejection fraction. Chronotropic function is primarily assessed using electrocardiograms (ECG) and Holter monitoring to analyze heart rate variability and rhythm in response to physiological stress or pharmacologic agents.
Summary: Clinical Implications and Future Directions
Inotropic agents primarily influence myocardial contractility, enhancing cardiac output in heart failure patients, while chronotropic agents adjust heart rate to manage arrhythmias and bradycardia. Understanding the differential effects allows for targeted therapy in conditions such as systolic dysfunction or sinus node dysfunction, optimizing cardiovascular function. Emerging research on combined inotropic-chronotropic modulators and gene therapy holds promise for personalized treatment strategies in complex cardiac disorders.
Inotropic Infographic
 libterm.com
libterm.com