Infections occur when harmful microorganisms such as bacteria, viruses, or fungi invade the body, triggering a response from the immune system. Symptoms can vary widely depending on the pathogen and the site of infection, ranging from mild discomfort to severe illness. Explore the full article to understand how infections spread, prevention tips, and treatment options that can protect your health.
Table of Comparison
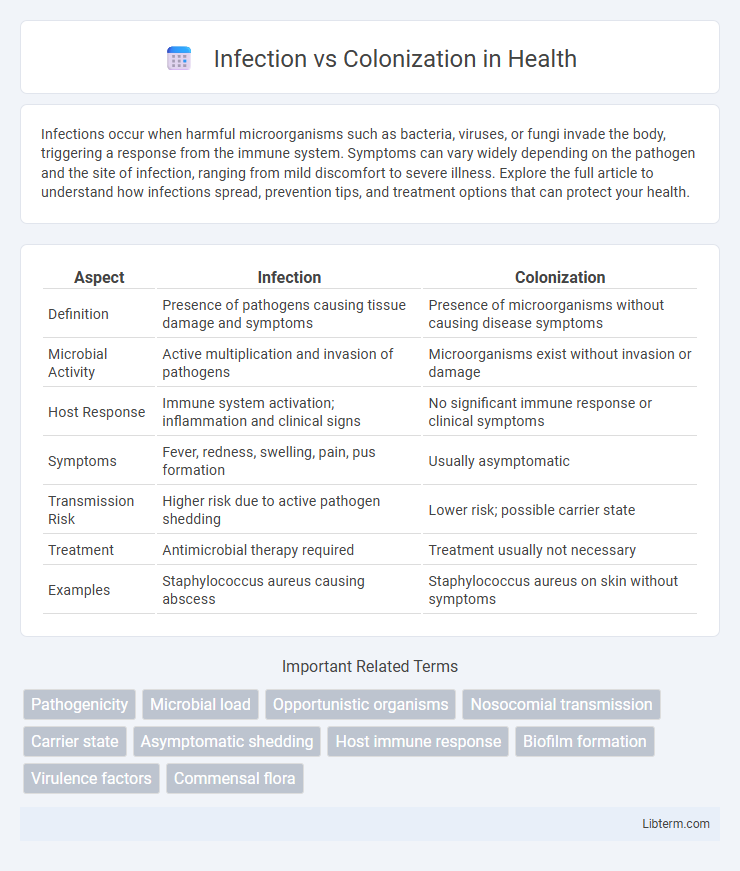
| Aspect | Infection | Colonization |
|---|---|---|
| Definition | Presence of pathogens causing tissue damage and symptoms | Presence of microorganisms without causing disease symptoms |
| Microbial Activity | Active multiplication and invasion of pathogens | Microorganisms exist without invasion or damage |
| Host Response | Immune system activation; inflammation and clinical signs | No significant immune response or clinical symptoms |
| Symptoms | Fever, redness, swelling, pain, pus formation | Usually asymptomatic |
| Transmission Risk | Higher risk due to active pathogen shedding | Lower risk; possible carrier state |
| Treatment | Antimicrobial therapy required | Treatment usually not necessary |
| Examples | Staphylococcus aureus causing abscess | Staphylococcus aureus on skin without symptoms |
Introduction: Understanding Infection vs Colonization
Infection occurs when pathogenic microorganisms invade body tissues, multiply, and trigger an immune response, often resulting in clinical symptoms. Colonization, by contrast, involves the presence of microbes on or within host surfaces without causing tissue damage or immune activation. Differentiating between infection and colonization is crucial for accurate diagnosis and appropriate antimicrobial therapy, minimizing unnecessary treatments and antibiotic resistance.
Definitions: What is Infection? What is Colonization?
Infection occurs when pathogenic microorganisms invade body tissues, causing an immune response and clinical symptoms, potentially leading to illness. Colonization refers to the presence of microorganisms on or within a host without causing tissue damage or symptoms, often serving as a reservoir for potential transmission. Understanding the distinction helps guide appropriate clinical management and infection control strategies.
Key Differences Between Infection and Colonization
Infection involves the invasion and multiplication of pathogenic microorganisms in body tissues causing clinical symptoms and an immune response, whereas colonization refers to the presence of microorganisms on or within the body without causing disease or symptoms. Infection typically results in tissue damage, inflammation, and systemic effects, while colonization is asymptomatic and may serve as a reservoir for potential pathogens. Laboratory tests showing active immune markers, elevated white blood cell counts, or positive cultures with corresponding clinical signs help distinguish infection from colonization.
Pathogenic Mechanisms: How Infection and Colonization Occur
Colonization occurs when microorganisms establish themselves on host surfaces without causing tissue damage, relying on adherence factors such as pili and biofilm formation to persist. Infection involves microbial invasion beyond barriers, triggering host immune responses through virulence factors like toxins, enzymes, and evasion strategies that facilitate tissue invasion and damage. Pathogenic mechanisms differentiate infection from colonization by the presence of active tissue injury and inflammation driven by microbial invasion and host-pathogen interactions.
Common Examples of Colonization and Infection
Staphylococcus aureus commonly colonizes the nasal passages and skin without causing disease, while its infection can lead to conditions like abscesses or pneumonia. Escherichia coli often colonizes the gastrointestinal tract harmlessly but causes infections such as urinary tract infections when it invades sterile sites. Candida species typically colonize mucosal surfaces like the mouth and vagina; however, overgrowth or immune suppression can result in invasive candidiasis or thrush.
Clinical Manifestations: Symptoms and Signs
Infection presents with clinical manifestations such as fever, localized pain, swelling, redness, and purulent discharge, indicating active tissue invasion and immune response. Colonization typically lacks these symptoms and shows the presence of microorganisms on mucosal or skin surfaces without causing inflammation or tissue damage. Laboratory findings in infection often reveal elevated white blood cell counts and positive cultures from sterile body sites, while colonization yields microbial growth without systemic or localized inflammatory signs.
Diagnosis: Differentiating Infection from Colonization
Accurate diagnosis differentiates infection from colonization by evaluating clinical symptoms, laboratory data, and microbiological findings. Infection is indicated by signs of host tissue damage, systemic response, and positive cultures in sterile sites, whereas colonization involves microorganism presence without host damage or symptoms. Biomarkers such as procalcitonin, along with imaging and patient history, support clinical judgment in distinguishing true infection from mere colonization.
Implications for Treatment and Management
Infection requires targeted antimicrobial therapy to eradicate the pathogenic microorganisms causing tissue damage, while colonization typically does not necessitate treatment as it involves presence of microbes without harmful effects. Accurate differentiation between infection and colonization is critical to avoid unnecessary antibiotic use, reducing the risk of antibiotic resistance development and adverse drug reactions. Effective management strategies incorporate clinical evaluation, microbiological data, and biomarkers to guide appropriate treatment decisions and optimize patient outcomes.
Impact on Infection Control and Prevention
Infection involves the invasion and multiplication of pathogens causing tissue damage and clinical symptoms, whereas colonization refers to the presence of microorganisms without causing disease. Effective infection control and prevention strategies prioritize distinguishing between infection and colonization to avoid unnecessary antibiotic use and reduce antimicrobial resistance. Surveillance, accurate diagnostic testing, and targeted isolation protocols are essential to limit the spread of infectious agents in healthcare settings while managing colonized patients safely.
Conclusion: Importance of Distinguishing Infection from Colonization
Distinguishing infection from colonization is crucial for accurate diagnosis and appropriate treatment, preventing unnecessary antibiotic use that contributes to resistance. Infection involves active microbial invasion causing symptoms, whereas colonization refers to the presence of microbes without tissue damage or clinical signs. Proper differentiation ensures targeted therapy, improves patient outcomes, and supports antimicrobial stewardship efforts.
Infection Infographic
 libterm.com
libterm.com