Thrombosis occurs when a blood clot forms inside a blood vessel, obstructing the flow of blood through the circulatory system and potentially causing serious health complications like stroke or pulmonary embolism. Understanding the causes, symptoms, and treatment options is essential for effective prevention and management. Explore the rest of the article to learn how you can recognize and reduce the risk of thrombosis.
Table of Comparison
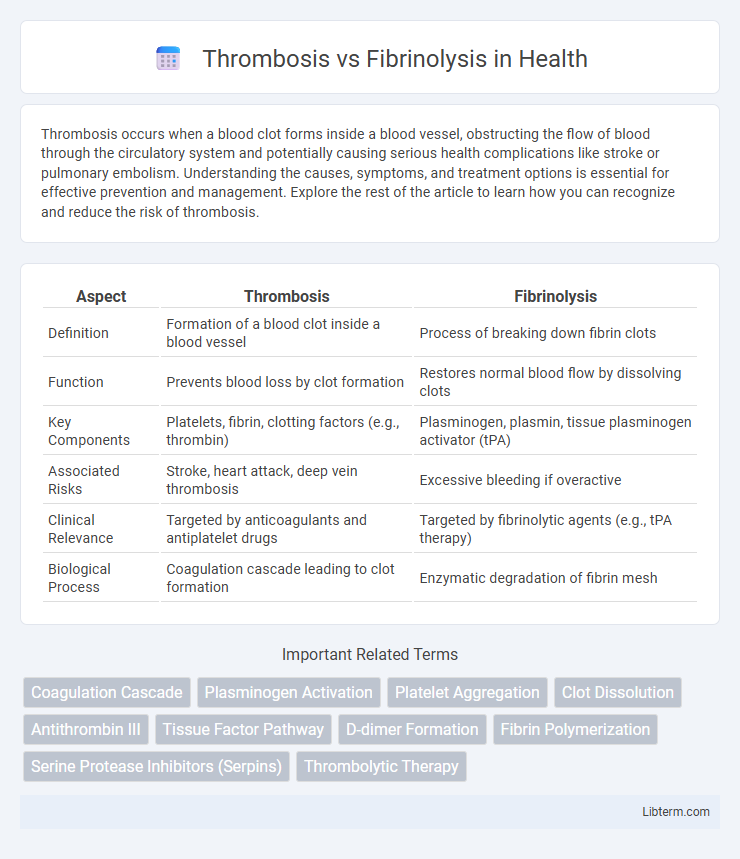
| Aspect | Thrombosis | Fibrinolysis |
|---|---|---|
| Definition | Formation of a blood clot inside a blood vessel | Process of breaking down fibrin clots |
| Function | Prevents blood loss by clot formation | Restores normal blood flow by dissolving clots |
| Key Components | Platelets, fibrin, clotting factors (e.g., thrombin) | Plasminogen, plasmin, tissue plasminogen activator (tPA) |
| Associated Risks | Stroke, heart attack, deep vein thrombosis | Excessive bleeding if overactive |
| Clinical Relevance | Targeted by anticoagulants and antiplatelet drugs | Targeted by fibrinolytic agents (e.g., tPA therapy) |
| Biological Process | Coagulation cascade leading to clot formation | Enzymatic degradation of fibrin mesh |
Introduction to Thrombosis and Fibrinolysis
Thrombosis is the pathological formation of blood clots within blood vessels, which can obstruct normal blood flow and lead to conditions such as stroke, myocardial infarction, and deep vein thrombosis. Fibrinolysis is the physiological process that breaks down fibrin clots through the activation of plasmin, restoring vessel patency and preventing excessive clot formation. The balance between thrombosis and fibrinolysis is critical for maintaining hemostatic equilibrium and preventing thrombotic or bleeding disorders.
What Is Thrombosis?
Thrombosis is the pathological formation of a blood clot within a blood vessel, obstructing normal blood flow and potentially leading to serious conditions such as stroke, myocardial infarction, or deep vein thrombosis. It involves the activation of platelets and the coagulation cascade, resulting in fibrin mesh stabilization that seals the site of vascular injury. Understanding thrombosis is crucial for managing cardiovascular diseases and developing therapies that target abnormal clot formation.
What Is Fibrinolysis?
Fibrinolysis is the biological process that breaks down blood clots by enzymatically degrading fibrin, the protein mesh that stabilizes thrombi during thrombosis. This mechanism is primarily facilitated by plasmin, an active enzyme derived from plasminogen, which dissolves fibrin strands to restore normal blood flow and prevent vessel occlusion. Impaired fibrinolysis can lead to excessive clot persistence, increasing the risk of thrombotic disorders such as stroke or deep vein thrombosis.
Key Differences: Thrombosis vs Fibrinolysis
Thrombosis involves the formation of a blood clot within a blood vessel, which can obstruct blood flow and lead to conditions like stroke or deep vein thrombosis. Fibrinolysis is the physiological process that breaks down clots by degrading fibrin, thus preventing excessive clotting and maintaining vascular patency. Key differences include thrombosis being a pathological clot formation, whereas fibrinolysis is a protective mechanism that ensures clot removal and tissue perfusion.
Mechanisms Behind Thrombosis Formation
Thrombosis formation involves the activation of platelets and the coagulation cascade, leading to the deposition of fibrin and the creation of a stable blood clot within a vessel. Endothelial injury triggers the exposure of tissue factor, initiating the extrinsic pathway, while platelet adhesion and aggregation amplify clot growth. Dysregulation of this process, such as excessive platelet activation or endothelial dysfunction, contributes to pathological thrombus development, contrasting with fibrinolysis, which enzymatically degrades fibrin to resolve clots.
Mechanisms of Fibrinolysis Activation
Fibrinolysis activation primarily involves the conversion of plasminogen to plasmin by tissue plasminogen activator (tPA) and urokinase plasminogen activator (uPA), which then degrades fibrin clots. This enzymatic process is tightly regulated by inhibitors such as plasminogen activator inhibitor-1 (PAI-1) and a2-antiplasmin to balance clot dissolution with hemostasis. Understanding these molecular mechanisms is crucial for therapeutic strategies targeting thrombotic disorders and enhancing fibrinolytic activity.
Risk Factors for Thrombosis and Impaired Fibrinolysis
Thrombosis risk factors include inherited conditions like factor V Leiden mutation, acquired factors such as prolonged immobility, surgery, cancer, and use of oral contraceptives, all of which promote excessive clot formation. Impaired fibrinolysis, marked by reduced plasmin activity or decreased levels of tissue plasminogen activator (tPA), hinders clot breakdown and contributes to persistent thrombi. Chronic inflammation and elevated levels of plasminogen activator inhibitor-1 (PAI-1) also exacerbate the imbalance between thrombosis and fibrinolysis, increasing cardiovascular and venous thromboembolism risk.
Clinical Implications and Consequences
Thrombosis, characterized by excessive clot formation, can obstruct blood vessels leading to myocardial infarction, stroke, or venous thromboembolism, while fibrinolysis serves as a critical physiological process that dissolves clots to restore hemostatic balance. Impaired fibrinolysis contributes to persistent thrombus presence and increased risk of ischemic events, whereas hyperactive fibrinolysis may result in bleeding complications. Understanding the dynamic interplay between thrombosis and fibrinolysis is essential for developing targeted anticoagulant and thrombolytic therapies in clinical practice.
Diagnostic Approaches: Thrombosis vs Fibrinolysis
Diagnostic approaches for thrombosis primarily involve imaging techniques such as Doppler ultrasound, venography, and MRI to detect blood clots in veins or arteries. In contrast, fibrinolysis assessment centers on laboratory tests measuring plasma levels of plasminogen activators, D-dimer, and fibrin degradation products, which indicate clot breakdown activity. Understanding the balance between thrombus formation and fibrinolytic activity is critical for accurate diagnosis and effective treatment planning.
Prevention and Treatment Strategies
Effective prevention of thrombosis includes the use of anticoagulants such as heparin and warfarin, as well as lifestyle modifications like regular exercise and smoking cessation to reduce clot formation. Fibrinolysis is enhanced through the administration of thrombolytic agents like tissue plasminogen activator (tPA), which accelerate the breakdown of fibrin clots and restore normal blood flow. Monitoring coagulation parameters and timely intervention with antiplatelet drugs also play crucial roles in managing the balance between thrombosis and fibrinolysis to prevent complications such as stroke or deep vein thrombosis.
Thrombosis Infographic
 libterm.com
libterm.com