A brain abscess is a serious infection characterized by a localized collection of pus within the brain tissue, often caused by bacteria or fungi. Symptoms may include headache, fever, neurological deficits, and changes in mental status, requiring prompt diagnosis through imaging techniques like MRI or CT scans. Discover essential information on causes, symptoms, treatment options, and how you can manage risks by reading the rest of this article.
Table of Comparison
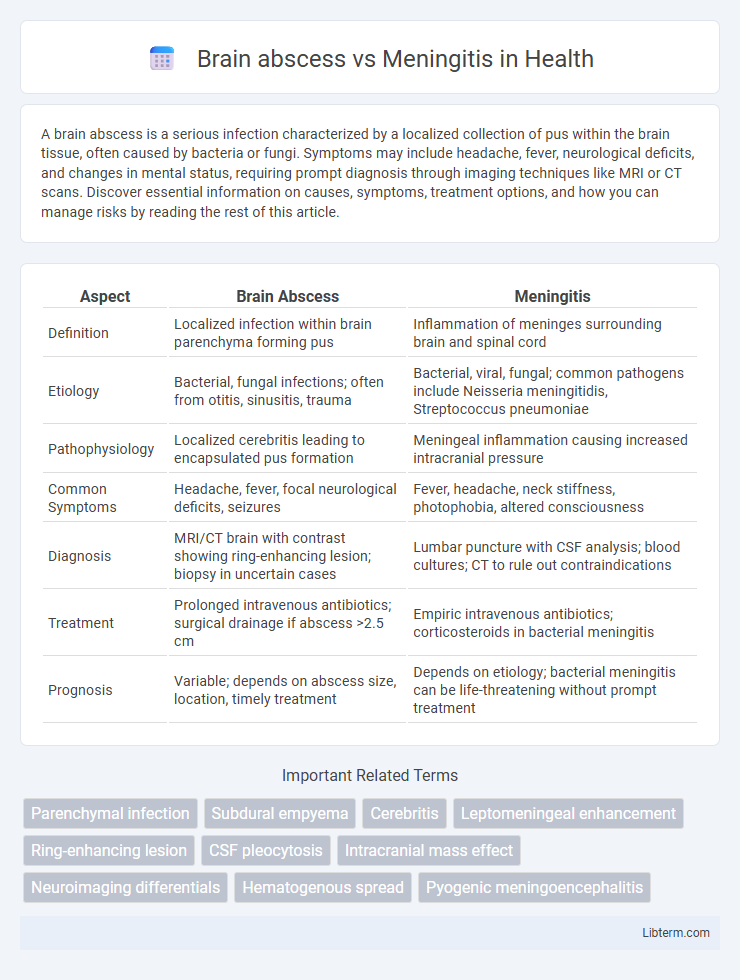
| Aspect | Brain Abscess | Meningitis |
|---|---|---|
| Definition | Localized infection within brain parenchyma forming pus | Inflammation of meninges surrounding brain and spinal cord |
| Etiology | Bacterial, fungal infections; often from otitis, sinusitis, trauma | Bacterial, viral, fungal; common pathogens include Neisseria meningitidis, Streptococcus pneumoniae |
| Pathophysiology | Localized cerebritis leading to encapsulated pus formation | Meningeal inflammation causing increased intracranial pressure |
| Common Symptoms | Headache, fever, focal neurological deficits, seizures | Fever, headache, neck stiffness, photophobia, altered consciousness |
| Diagnosis | MRI/CT brain with contrast showing ring-enhancing lesion; biopsy in uncertain cases | Lumbar puncture with CSF analysis; blood cultures; CT to rule out contraindications |
| Treatment | Prolonged intravenous antibiotics; surgical drainage if abscess >2.5 cm | Empiric intravenous antibiotics; corticosteroids in bacterial meningitis |
| Prognosis | Variable; depends on abscess size, location, timely treatment | Depends on etiology; bacterial meningitis can be life-threatening without prompt treatment |
Introduction to Brain Abscess and Meningitis
Brain abscess is a localized collection of pus within the brain parenchyma, caused by bacterial or fungal infections, leading to inflammation and increased intracranial pressure. Meningitis involves inflammation of the meninges, the protective membranes covering the brain and spinal cord, often resulting from viral, bacterial, or fungal pathogens. Both conditions require prompt diagnosis and treatment due to their potential to cause severe neurological damage and systemic complications.
Definition and Overview
A brain abscess is a localized collection of pus within the brain tissue caused by infection, often bacterial or fungal, leading to inflammation and increased intracranial pressure. Meningitis is the inflammation of the protective membranes covering the brain and spinal cord, typically resulting from bacterial, viral, or fungal infections. Both conditions require prompt diagnosis and treatment but differ in their anatomical location and pathological impact.
Causes and Risk Factors
Brain abscesses typically result from bacterial or fungal infections spreading from nearby structures such as sinusitis, otitis media, or through hematogenous dissemination from distant infections, with risk factors including immunocompromised states, chronic ear or sinus infections, and head trauma. Meningitis is primarily caused by viral, bacterial, or fungal pathogens invading the meninges, often due to close contact with infected individuals, compromised immune defenses, or conditions like cerebrospinal fluid leaks and neurosurgical procedures. Both conditions share overlapping risk factors such as immunosuppression but differ in the primary infection sites and pathways of pathogen entry.
Pathophysiology: How Each Condition Develops
Brain abscess develops as a localized collection of pus within the brain tissue, typically resulting from bacterial or fungal infection spreading from adjacent structures, hematogenous dissemination, or direct inoculation following trauma or surgery. The infectious agents trigger an inflammatory response, leading to necrosis, edema, and capsule formation around the abscess to contain the infection. Meningitis involves inflammation of the meninges caused by bacterial, viral, or fungal pathogens invading the subarachnoid space, provoking an immune response that increases vascular permeability, results in meningeal edema, and disrupts cerebrospinal fluid circulation.
Key Differences in Clinical Presentation
Brain abscess typically presents with localized neurological deficits, headache, fever, and signs of increased intracranial pressure such as vomiting and papilledema. Meningitis often manifests with fever, neck stiffness, photophobia, and altered mental status due to meningeal inflammation. Unlike meningitis, brain abscess may show focal signs on imaging and progress more gradually, whereas meningitis generally has an acute onset with systemic symptoms.
Diagnostic Approaches and Tools
Brain abscess diagnosis involves magnetic resonance imaging (MRI) with contrast and computed tomography (CT) scans to detect localized pus accumulation and ring-enhancing lesions, while lumbar puncture is contraindicated due to risk of herniation. Meningitis diagnosis relies heavily on cerebrospinal fluid (CSF) analysis obtained through lumbar puncture, assessing cell count, glucose, protein, and culture to identify inflammation and causative pathogens. Advanced molecular techniques such as polymerase chain reaction (PCR) assays enhance pathogen detection accuracy in both conditions, improving differential diagnosis and guiding targeted treatment.
Treatment Modalities for Brain Abscess
Treatment modalities for brain abscess primarily include surgical intervention such as aspiration or excision to remove the abscess, combined with prolonged intravenous antibiotic therapy targeting common pathogens like Streptococcus, Staphylococcus, and anaerobes. Empiric antibiotic regimens often consist of a combination of third-generation cephalosporins, metronidazole, and vancomycin until culture results guide specific therapy. Adjunctive measures may involve corticosteroids to reduce cerebral edema and anticonvulsants to prevent seizures, emphasizing individualized management based on abscess size, location, and patient clinical status.
Therapeutic Options for Meningitis
Therapeutic options for meningitis primarily include prompt administration of intravenous antibiotics tailored to the suspected or confirmed pathogen, with common choices like ceftriaxone or vancomycin for bacterial meningitis. Adjunctive corticosteroids, such as dexamethasone, are often used to reduce inflammation and prevent neurological complications. Supportive care involves managing symptoms, maintaining fluid balance, and monitoring for potential complications such as increased intracranial pressure or seizures.
Prognosis and Potential Complications
Brain abscess prognosis depends on early diagnosis and treatment, with potential complications including increased intracranial pressure, seizures, and neurological deficits. Meningitis prognosis varies by causative pathogen, with bacterial meningitis posing a higher risk of mortality and complications like hearing loss, cognitive impairment, and stroke. Both conditions require prompt intervention to reduce morbidity and improve patient outcomes.
Prevention Strategies and Patient Education
Effective prevention strategies for brain abscess include proper management of infections such as otitis media, sinusitis, and dental abscesses, along with prompt treatment of immunocompromised conditions to reduce hematogenous spread. Meningitis prevention emphasizes vaccination against common pathogens like Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae type b, as well as maintaining hygiene practices to prevent respiratory droplet transmission. Educating patients on recognizing early symptoms, adhering to vaccination schedules, and seeking immediate medical care for infections significantly reduces morbidity and mortality associated with both conditions.
Brain abscess Infographic
 libterm.com
libterm.com