Necrosis is the premature death of cells and living tissue caused by injury, infection, or lack of blood supply, leading to inflammation and tissue damage. This process disrupts normal cellular function and can result in severe complications if not treated promptly. Discover how to recognize, prevent, and manage necrosis to protect your health by reading the full article.
Table of Comparison
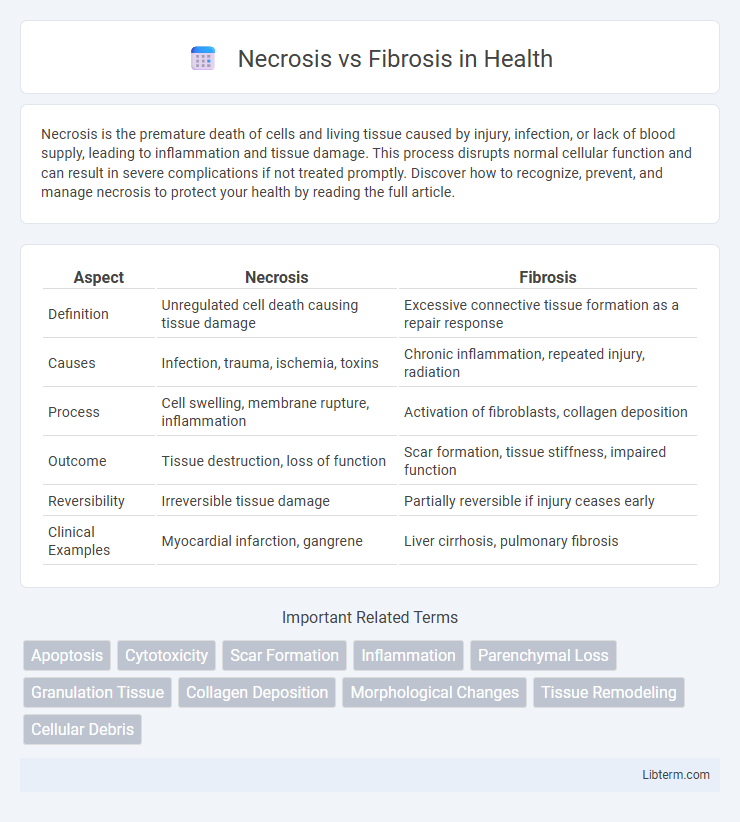
| Aspect | Necrosis | Fibrosis |
|---|---|---|
| Definition | Unregulated cell death causing tissue damage | Excessive connective tissue formation as a repair response |
| Causes | Infection, trauma, ischemia, toxins | Chronic inflammation, repeated injury, radiation |
| Process | Cell swelling, membrane rupture, inflammation | Activation of fibroblasts, collagen deposition |
| Outcome | Tissue destruction, loss of function | Scar formation, tissue stiffness, impaired function |
| Reversibility | Irreversible tissue damage | Partially reversible if injury ceases early |
| Clinical Examples | Myocardial infarction, gangrene | Liver cirrhosis, pulmonary fibrosis |
Introduction to Necrosis and Fibrosis
Necrosis is the pathological process of cell death caused by external factors such as injury, infection, or toxins, resulting in the uncontrolled breakdown of cellular components. Fibrosis refers to the excessive accumulation of extracellular matrix proteins, particularly collagen, leading to tissue scarring and impaired organ function after chronic injury or inflammation. Both necrosis and fibrosis play crucial roles in disease progression by disrupting normal tissue architecture and homeostasis.
Definition of Necrosis
Necrosis is the pathological process of cell death caused by factors such as ischemia, toxins, or trauma, resulting in the unregulated digestion of cell components and loss of membrane integrity. Unlike apoptosis, necrosis leads to inflammation and tissue damage due to the release of intracellular contents. Fibrosis, by contrast, involves the excessive buildup of extracellular matrix proteins, often as a reparative response to chronic injury or persistent inflammation.
Definition of Fibrosis
Fibrosis is the pathological accumulation of excess extracellular matrix components, primarily collagen, leading to the thickening and scarring of connective tissue in organs. Unlike necrosis, which involves the premature death of cells causing tissue damage, fibrosis represents a chronic, reparative process that results in tissue stiffening and loss of function. This excessive fibrotic response often occurs after injury or inflammation, contributing to diseases such as pulmonary fibrosis, liver cirrhosis, and cardiac fibrosis.
Key Differences Between Necrosis and Fibrosis
Necrosis involves the uncontrolled death of cells due to injury or disease, characterized by cell membrane rupture and inflammation, whereas fibrosis is the excessive accumulation of extracellular matrix proteins leading to tissue scarring and impaired function. Necrosis results in tissue damage and triggers an inflammatory response, while fibrosis represents a chronic repair process that replaces normal tissue with fibrotic scar tissue. These conditions differ fundamentally in pathology, with necrosis being a destructive event and fibrosis a progressive remodeling outcome.
Causes of Necrosis
Necrosis results from factors such as ischemia, infections, toxins, and trauma leading to uncontrolled cell death. In contrast, fibrosis involves the excessive accumulation of extracellular matrix proteins during chronic inflammation or tissue repair. Understanding the distinct causes and mechanisms of necrosis is crucial for diagnosing and treating tissue damage effectively.
Causes of Fibrosis
Fibrosis is primarily caused by chronic tissue injury that triggers excessive extracellular matrix production and scarring, often resulting from persistent inflammation, infection, or autoimmune diseases. Unlike necrosis, which involves acute cell death due to factors such as ischemia or toxins, fibrosis develops through sustained damage and abnormal wound healing processes. Key molecular drivers include activation of fibroblasts, transforming growth factor-beta (TGF-b), and other profibrotic cytokines that promote collagen deposition and tissue remodeling.
Pathophysiological Mechanisms
Necrosis involves uncontrolled cell death triggered by factors such as ischemia, toxins, or trauma, leading to the release of intracellular contents and subsequent inflammation. Fibrosis is characterized by the excessive accumulation of extracellular matrix proteins, primarily collagen, due to chronic injury or inflammation, resulting in tissue scarring and altered organ function. The pathophysiological mechanisms diverge as necrosis causes acute tissue damage and inflammation, whereas fibrosis represents a maladaptive repair process driven by activated fibroblasts and persistent profibrotic signaling pathways like TGF-b.
Clinical Manifestations
Necrosis presents with clinical manifestations such as localized pain, swelling, redness, and loss of function, often accompanied by systemic symptoms like fever and malaise when infection is involved. Fibrosis typically manifests as tissue stiffness, reduced elasticity, and impaired organ function, with symptoms depending on the affected organ, such as respiratory difficulty in pulmonary fibrosis or cirrhosis in hepatic fibrosis. Both conditions can lead to chronic complications, but necrosis is primarily associated with acute tissue damage, whereas fibrosis reflects a chronic reparative or pathological scarring process.
Diagnostic Approaches
Diagnostic approaches for distinguishing necrosis from fibrosis primarily involve histopathological examination through biopsy, where necrosis is identified by cell death and tissue breakdown, while fibrosis shows excess collagen deposition and scar tissue formation. Imaging techniques such as MRI and CT scans can reveal structural differences, with necrosis often appearing as areas of hypodensity or signal voids due to cell death, and fibrosis manifesting as dense, fibrotic regions with altered tissue architecture. Biomarkers like elevated lactate dehydrogenase (LDH) levels suggest necrosis, whereas increased collagen markers such as pro-collagen peptides are indicative of fibrosis presence.
Treatment and Management Strategies
Treatment of necrosis primarily involves removing the dead tissue through surgical debridement to prevent infection and promote healing, supplemented by antibiotics if infection is suspected. Management of fibrosis centers on controlling inflammation and preventing scar tissue formation using anti-inflammatory medications, antifibrotic agents such as pirfenidone or nintedanib, and physical therapy to maintain tissue function. Early diagnosis and targeted therapy are crucial in both conditions to minimize complications and improve patient outcomes.
Necrosis Infographic
 libterm.com
libterm.com