Hyponatremia occurs when your blood sodium levels drop below normal, disrupting cellular function and causing symptoms like nausea, headaches, and confusion. It can result from conditions such as heart failure, kidney disease, or excessive fluid intake. Explore the rest of the article to understand the causes, symptoms, and effective treatments for hyponatremia.
Table of Comparison
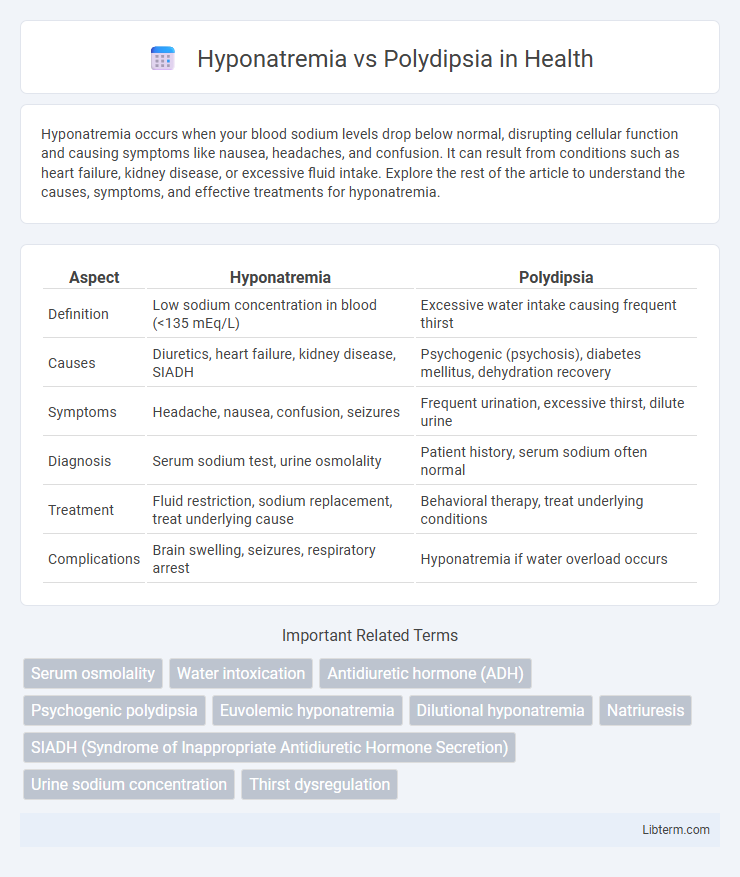
| Aspect | Hyponatremia | Polydipsia |
|---|---|---|
| Definition | Low sodium concentration in blood (<135 mEq/L) | Excessive water intake causing frequent thirst |
| Causes | Diuretics, heart failure, kidney disease, SIADH | Psychogenic (psychosis), diabetes mellitus, dehydration recovery |
| Symptoms | Headache, nausea, confusion, seizures | Frequent urination, excessive thirst, dilute urine |
| Diagnosis | Serum sodium test, urine osmolality | Patient history, serum sodium often normal |
| Treatment | Fluid restriction, sodium replacement, treat underlying cause | Behavioral therapy, treat underlying conditions |
| Complications | Brain swelling, seizures, respiratory arrest | Hyponatremia if water overload occurs |
Understanding Hyponatremia: Definition and Causes
Hyponatremia is a medical condition characterized by low sodium levels in the blood, often caused by excessive water intake, kidney dysfunction, or hormonal imbalances. Polydipsia, an abnormal craving for water, can lead to dilutional hyponatremia by overwhelming the body's ability to maintain electrolyte balance. Understanding the underlying causes of hyponatremia, including psychiatric polydipsia and renal issues, is critical for accurate diagnosis and effective treatment.
What is Polydipsia? Overview and Key Differences
Polydipsia is characterized by excessive thirst and fluid intake, often linked to underlying conditions like diabetes mellitus or psychogenic origins. Hyponatremia occurs when the sodium concentration in the blood falls below 135 mmol/L, frequently due to water overload from polydipsia causing dilutional hyponatremia. The key difference lies in polydipsia as a symptom related to increased water consumption, while hyponatremia is a biochemical imbalance that can result from excessive fluid intake or impaired sodium regulation.
Pathophysiology: How Hyponatremia Develops
Hyponatremia develops when the body retains excess water relative to sodium, leading to diluted serum sodium levels below 135 mmol/L. This imbalance often results from inappropriate antidiuretic hormone (ADH) secretion or excessive free water intake, as seen in polydipsia, where overconsumption of fluids overwhelms renal capacity to excrete water. The resulting hypoosmolar state causes cellular swelling, particularly in the brain, contributing to neurological symptoms.
Types and Triggers of Polydipsia
Polydipsia manifests primarily in two types: primary polydipsia, which is driven by excessive fluid intake often triggered by psychological factors such as stress or schizophrenia, and secondary polydipsia, which occurs due to physiological causes like uncontrolled diabetes mellitus or diuretic use. Differentiating polydipsia-induced hyponatremia from other causes necessitates understanding these triggers, since excessive water intake dilutes serum sodium levels, leading to hyponatremia. Effective management depends on identifying whether polydipsia stems from psychogenic behaviors or secondary medical conditions to tailor appropriate interventions.
Clinical Symptoms: Comparing Hyponatremia and Polydipsia
Hyponatremia typically presents with symptoms such as nausea, headache, confusion, seizures, and in severe cases, coma due to low sodium levels disrupting neuronal function. Polydipsia, characterized by excessive water intake, often leads to dilutional hyponatremia, presenting with similar neurological symptoms but is distinguished by thirst and excessive urination. Differentiating these conditions relies on evaluating sodium concentration, fluid intake history, and associated clinical features like altered mental status and volume status.
Diagnostic Criteria: Lab Tests and Assessment
Hyponatremia diagnosis involves measuring serum sodium levels below 135 mEq/L, assessing serum osmolality, urine sodium concentration, and urine osmolality to distinguish causes such as SIADH or volume depletion. Polydipsia diagnosis requires evaluation of excessive fluid intake with corresponding low urine osmolality and high urine volume, often confirmed by water deprivation tests and serum electrolyte assessment to rule out disorders like diabetes insipidus. Accurate differentiation relies on comprehensive lab testing including serum sodium, plasma osmolality, urine osmolality, and clinical history of fluid intake patterns.
Risk Factors and At-Risk Populations
Hyponatremia commonly affects elderly patients, individuals with congestive heart failure, liver cirrhosis, and those using diuretics or selective serotonin reuptake inhibitors (SSRIs), increasing their risk due to electrolyte imbalances. Polydipsia is frequently observed in psychiatric populations, particularly patients with schizophrenia or anxiety disorders, who may consume excessive water leading to dilutional hyponatremia. Both conditions have heightened prevalence in hospitalized or institutionalized patients, making careful monitoring essential to prevent severe neurological complications.
Treatment Options: Managing Hyponatremia vs. Polydipsia
Hyponatremia treatment focuses on carefully correcting sodium levels through fluid restriction, saline infusions, or medications like demeclocycline to prevent rapid shifts in serum sodium and avoid osmotic demyelination syndrome. Managing polydipsia involves behavioral interventions to limit water intake, addressing underlying psychiatric conditions, and monitoring electrolytes to prevent dilutional hyponatremia. Both conditions require tailored approaches to safely restore electrolyte balance and prevent complications.
Potential Complications and Prognosis
Hyponatremia, characterized by low serum sodium levels, can lead to severe neurological complications such as seizures, cerebral edema, and even coma if left untreated. Polydipsia-induced hyponatremia, often seen in chronic psychiatric conditions, results from excessive water intake overwhelming the kidneys' ability to excrete water, increasing the risk of osmotic imbalance and water intoxication. Early diagnosis and careful management of sodium levels are critical to improving prognosis and preventing long-term cognitive impairment or fatal outcomes.
Prevention Strategies and Patient Education
Effective prevention of hyponatremia in patients with polydipsia involves educating individuals to regulate fluid intake and recognize early symptoms of electrolyte imbalance such as headache and confusion. Healthcare providers should emphasize the importance of monitoring daily fluid consumption, advising patients to avoid excessive water intake beyond recommended limits, particularly in psychiatric populations prone to psychogenic polydipsia. Patient education also includes instruction on maintaining a balanced diet rich in sodium and seeking prompt medical evaluation for symptoms indicative of hyponatremia to prevent severe neurological complications.
Hyponatremia Infographic
 libterm.com
libterm.com