Sialadenitis is the inflammation of the salivary glands, often caused by bacterial or viral infections, while sialolithiasis refers to the formation of salivary gland stones blocking saliva flow. Both conditions can lead to swelling, pain, and difficulty in swallowing, posing discomfort and potential complications if untreated. Discover more detailed information on symptoms, causes, and effective treatments for your oral health in the rest of this article.
Table of Comparison
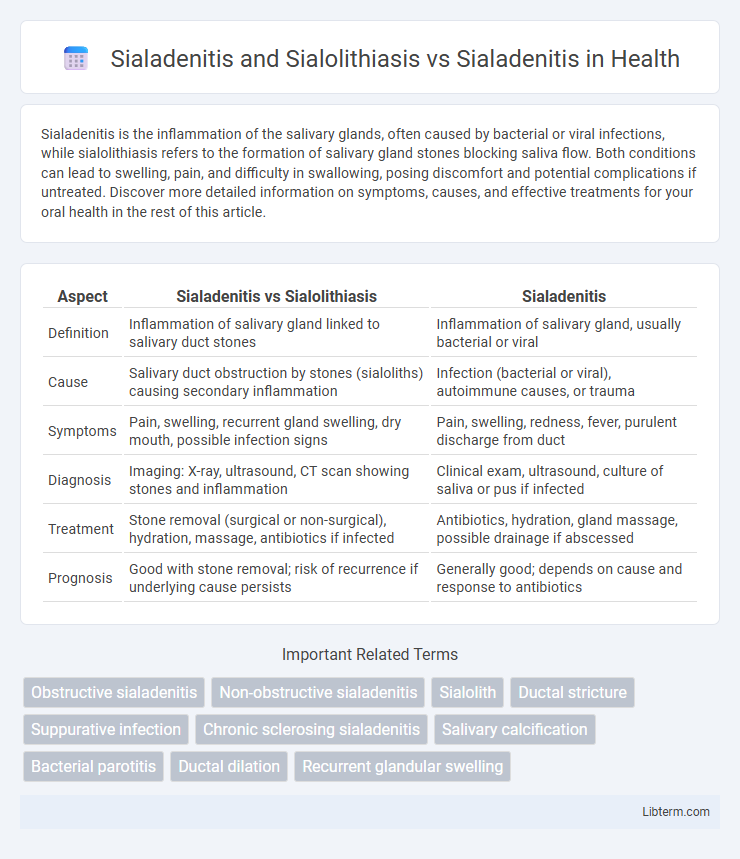
| Aspect | Sialadenitis vs Sialolithiasis | Sialadenitis |
|---|---|---|
| Definition | Inflammation of salivary gland linked to salivary duct stones | Inflammation of salivary gland, usually bacterial or viral |
| Cause | Salivary duct obstruction by stones (sialoliths) causing secondary inflammation | Infection (bacterial or viral), autoimmune causes, or trauma |
| Symptoms | Pain, swelling, recurrent gland swelling, dry mouth, possible infection signs | Pain, swelling, redness, fever, purulent discharge from duct |
| Diagnosis | Imaging: X-ray, ultrasound, CT scan showing stones and inflammation | Clinical exam, ultrasound, culture of saliva or pus if infected |
| Treatment | Stone removal (surgical or non-surgical), hydration, massage, antibiotics if infected | Antibiotics, hydration, gland massage, possible drainage if abscessed |
| Prognosis | Good with stone removal; risk of recurrence if underlying cause persists | Generally good; depends on cause and response to antibiotics |
Understanding Sialadenitis: Definition and Causes
Sialadenitis is an inflammatory condition affecting the salivary glands, commonly caused by bacterial infections, viral infections like mumps, or autoimmune diseases such as Sjogren's syndrome. Sialolithiasis, the formation of salivary gland stones, often leads to obstructive sialadenitis by blocking salivary flow and causing gland inflammation. Understanding these distinct causes highlights the importance of accurate diagnosis to differentiate primary inflammatory sialadenitis from those secondary to sialolithiasis for effective treatment.
Overview of Sialolithiasis: Formation and Risk Factors
Sialolithiasis involves the formation of calcified stones within the salivary glands, most commonly affecting the submandibular gland due to its viscous saliva and upward duct anatomy. Risk factors include dehydration, reduced salivary flow, chronic sialadenitis, and certain medications that decrease saliva production. These factors contribute to mineral precipitation around an organic nidus, leading to obstructive symptoms and secondary infection.
Pathophysiology: How Sialolithiasis Leads to Sialadenitis
Sialolithiasis causes obstruction of salivary gland ducts by calcified stones, leading to saliva stasis and increased intraductal pressure. This obstruction creates a conducive environment for bacterial infection, resulting in inflammation of the gland tissue, known as sialadenitis. The impaired salivary flow in sialolithiasis directly contributes to the pathophysiology of sialadenitis through ductal blockage and secondary infection.
Clinical Differences: Sialadenitis With and Without Sialolithiasis
Sialadenitis with sialolithiasis typically presents with acute, recurrent pain and swelling of the affected salivary gland, often exacerbated by meals due to obstruction caused by salivary stones. In contrast, sialadenitis without sialolithiasis usually manifests as diffuse gland enlargement and tenderness resulting from bacterial or viral infection without mechanical blockage. Fever, purulent ductal discharge, and localized erythema are more prominent in sialadenitis with sialolithiasis due to secondary infection from salivary stasis.
Signs and Symptoms: Comparative Analysis
Sialadenitis commonly presents with painful swelling and tenderness of the affected salivary gland, often accompanied by fever and purulent discharge from the duct, while sialolithiasis primarily causes intermittent glandular swelling and pain, especially during meals due to stone obstruction. In comparison to sialadenitis, sialadenitis with concurrent sialolithiasis tends to exhibit more acute pain localized near the obstruction site and may include visible ductal swelling or erythema. Both conditions share symptoms like gland enlargement and discomfort, but sialolithiasis is distinguished by obstructive features and episodic symptom patterns linked to salivary flow impairment.
Diagnostic Approaches: Sialadenitis vs. Sialolithiasis-associated Sialadenitis
Diagnostic approaches for sialadenitis typically involve clinical examination, ultrasonography, and salivary gland scintigraphy to assess gland inflammation and function, whereas sialolithiasis-associated sialadenitis requires precise imaging techniques such as cone-beam computed tomography (CBCT) or sialography to identify obstructive salivary duct stones. Ultrasonography is highly sensitive in detecting salivary gland swelling and ductal dilatation in sialadenitis, while sialolithiasis diagnosis benefits from high-resolution imaging to visualize calculi and evaluate ductal obstruction. Laboratory tests including leukocyte counts and culture of saliva may aid in confirming bacterial infection in both conditions but are more critical in sialadenitis without stones.
Imaging Techniques for Accurate Differentiation
Imaging techniques such as ultrasound, CT, and MRI play a crucial role in differentiating sialadenitis from sialolithiasis by identifying inflammation and obstruction within salivary glands. Ultrasound effectively reveals hypoechoic areas and ductal dilation in sialadenitis, while pinpointing echogenic stones with posterior shadowing characteristic of sialolithiasis. CT and MRI further enhance diagnostic accuracy by detecting glandular swelling, precise stone localization, and assessing soft tissue involvement to guide appropriate treatment.
Treatment Modalities: Isolated Sialadenitis vs. Sialolithiasis-induced Sialadenitis
Isolated sialadenitis treatment primarily involves hydration, warm compresses, gland massage, and broad-spectrum antibiotics to address bacterial infection. In contrast, sialolithiasis-induced sialadenitis requires additional interventions such as sialolith removal via sialendoscopy, extracorporeal shock wave lithotripsy, or surgical excision to alleviate duct obstruction and prevent recurrent infections. Supportive care remains essential in both conditions to reduce inflammation and restore salivary gland function.
Prognosis and Complications: Comparative Outcomes
Sialadenitis combined with sialolithiasis often results in recurrent gland obstruction and increased risk of chronic infection, leading to a comparatively guarded prognosis versus sialadenitis alone. Patients with sialolithiasis experience higher rates of glandular abscess formation and ductal fibrosis, contributing to long-term gland dysfunction. In contrast, sialadenitis without sialolithiasis generally resolves more rapidly with fewer complications when promptly treated.
Prevention and Long-term Management Strategies
Prevention of Sialadenitis and Sialolithiasis focuses on maintaining proper hydration, practicing good oral hygiene, and stimulating saliva flow through regular chewing of sugar-free gum to reduce the risk of salivary gland infection and stone formation. Long-term management strategies for Sialadenitis include antibiotics for bacterial infections, warm compresses, gland massage, and surgical intervention if necessary, while Sialolithiasis may require minimally invasive stone removal procedures or sialendoscopy to prevent recurrent gland inflammation. Regular dental check-ups and lifestyle modifications such as avoiding medications that cause dry mouth are critical to reducing recurrence and preserving salivary gland function.
Sialadenitis and Sialolithiasis Infographic
 libterm.com
libterm.com