Gynecomastia refers to the enlargement of glandular breast tissue in males, often caused by hormonal imbalances, whereas pseudogynecomastia results from excess fat deposits without glandular growth. Differentiating between these conditions is crucial for determining the appropriate treatment approach, which may include lifestyle changes, medication, or surgery. Explore the rest of the article to understand the causes, diagnosis, and treatment options tailored for your needs.
Table of Comparison
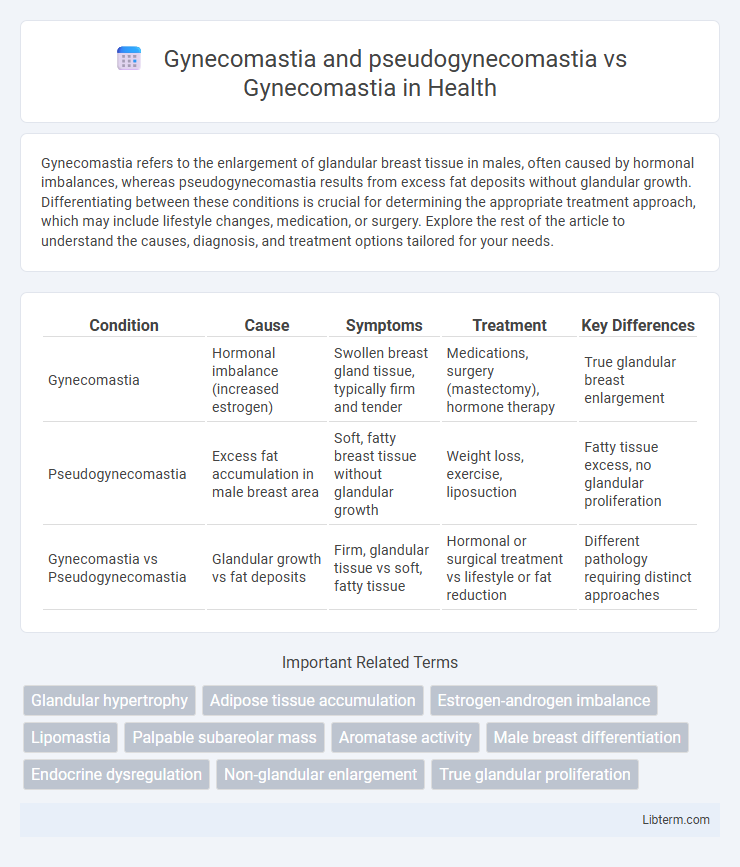
| Condition | Cause | Symptoms | Treatment | Key Differences |
|---|---|---|---|---|
| Gynecomastia | Hormonal imbalance (increased estrogen) | Swollen breast gland tissue, typically firm and tender | Medications, surgery (mastectomy), hormone therapy | True glandular breast enlargement |
| Pseudogynecomastia | Excess fat accumulation in male breast area | Soft, fatty breast tissue without glandular growth | Weight loss, exercise, liposuction | Fatty tissue excess, no glandular proliferation |
| Gynecomastia vs Pseudogynecomastia | Glandular growth vs fat deposits | Firm, glandular tissue vs soft, fatty tissue | Hormonal or surgical treatment vs lifestyle or fat reduction | Different pathology requiring distinct approaches |
Understanding Gynecomastia: Definition and Causes
Gynecomastia is the enlargement of male breast glandular tissue caused by hormonal imbalances, particularly an increased ratio of estrogen to testosterone. In contrast, pseudogynecomastia involves the accumulation of excess fat without glandular proliferation, often related to obesity. Recognizing these differences is crucial for effective diagnosis and treatment, as gynecomastia may require endocrine evaluation while pseudogynecomastia responds primarily to weight management.
What Is Pseudogynecomastia? Key Differences
Pseudogynecomastia is characterized by excess fat accumulation in the male breast area without the glandular tissue growth seen in true gynecomastia, which involves benign enlargement of male breast glandular tissue. Unlike gynecomastia, pseudogynecomastia results primarily from obesity or weight gain rather than hormonal imbalances or medication side effects. Key differences include the absence of firm glandular tissue under the nipple in pseudogynecomastia and treatment approaches focusing on weight loss for pseudogynecomastia versus medical or surgical intervention for gynecomastia.
Gynecomastia vs Pseudogynecomastia: Symptoms Comparison
Gynecomastia presents as a rubbery or firm mass extending concentrically from the nipples, often accompanied by tenderness or sensitivity, while pseudogynecomastia is characterized by diffuse, soft fatty tissue without a distinct mass or pain. In gynecomastia, glandular breast tissue proliferation is palpable beneath the nipple, whereas pseudogynecomastia involves increased subcutaneous fat deposition without true glandular enlargement. Distinguishing symptoms such as the presence of a firm, mobile glandular component versus soft adipose tissue help differentiate gynecomastia from pseudogynecomastia during clinical examination.
Hormonal Factors in Gynecomastia Development
Gynecomastia involves the enlargement of male breast tissue due to an imbalance between estrogen and androgen hormones, often triggered by increased estrogen levels or decreased testosterone production. Pseudogynecomastia, on the other hand, is characterized by fat accumulation without glandular proliferation and is not influenced by hormonal shifts. Understanding hormonal factors is critical in distinguishing true gynecomastia from pseudogynecomastia, as hormonal imbalances directly stimulate glandular breast tissue growth in gynecomastia development.
Risk Factors and Common Triggers
Gynecomastia is primarily caused by hormonal imbalances, particularly elevated estrogen or reduced testosterone levels, often triggered by puberty, aging, or certain medications like anti-androgens and steroids. Pseudogynecomastia results from excess fat deposition in the chest area without glandular proliferation, commonly linked to obesity, poor diet, and sedentary lifestyle. Risk factors for true gynecomastia include liver disease, testicular tumors, and endocrine disorders, whereas pseudogynecomastia is mainly associated with metabolic syndrome and weight gain.
Diagnostic Approaches for Male Breast Enlargement
Gynecomastia is characterized by a glandular breast tissue proliferation, whereas pseudogynecomastia results from excess adipose tissue without glandular growth. Diagnostic approaches for male breast enlargement include clinical examination, ultrasound imaging, and mammography to differentiate between glandular and fatty tissue. Hormonal assays and biopsy may be required in ambiguous cases to confirm the diagnosis and exclude malignancies.
Physical Examination: Differentiating Between Conditions
Physical examination is crucial in differentiating gynecomastia from pseudogynecomastia, with palpable glandular tissue beneath the nipple indicating true gynecomastia, whereas pseudogynecomastia presents with diffuse, soft fatty tissue without a firm mass. In true gynecomastia, the glandular tissue often feels rubbery or firm and is concentric to the nipple, while pseudogynecomastia typically shows no discrete mass and involves generalized chest fat deposition. Accurate clinical assessment helps guide further diagnostic evaluation and appropriate treatment strategies.
Treatment Options for Gynecomastia
Treatment options for gynecomastia primarily include medical therapy and surgical intervention, with liposuction and mastectomy being the most effective surgical approaches. Medical treatments often involve selective estrogen receptor modulators (SERMs) like tamoxifen or aromatase inhibitors to reduce glandular breast tissue, whereas pseudogynecomastia, characterized by excess fat without glandular proliferation, is best addressed through weight loss and liposuction. Accurate diagnosis differentiating true gynecomastia from pseudogynecomastia is crucial to choosing an appropriate treatment plan focused on tissue composition and severity.
Managing Pseudogynecomastia: Lifestyle and Medical Solutions
Managing pseudogynecomastia primarily involves targeted lifestyle changes such as a balanced diet, regular cardiovascular exercise, and strength training to reduce fatty tissue in the chest area. Medical approaches include consultations for potential liposuction or non-invasive fat reduction procedures like CoolSculpting, which specifically target adipose tissue without affecting glandular breast tissue seen in true gynecomastia. Differentiating pseudogynecomastia from gynecomastia is essential, as true gynecomastia may require hormone therapy or surgical glandular tissue removal for effective treatment.
Prevention Strategies and Long-Term Outlook
Prevention strategies for gynecomastia involve managing hormone levels by avoiding anabolic steroids, certain medications, and alcohol abuse, while pseudogynecomastia prevention focuses on maintaining a healthy weight through balanced diet and regular exercise. Long-term outlook for gynecomastia varies; some cases resolve spontaneously, but persistent or severe enlargement may require medical or surgical intervention, whereas pseudogynecomastia often improves with lifestyle modifications and weight loss. Early identification and tailored approaches ensure better management of both conditions, minimizing psychological and physical complications.
Gynecomastia and pseudogynecomastia Infographic
 libterm.com
libterm.com