Sepsis is a life-threatening condition caused by the body's extreme response to infection, which can lead to tissue damage, organ failure, and death if not treated promptly. Early recognition of symptoms like fever, rapid heartbeat, and confusion is crucial for improving outcomes and preventing complications. Discover essential information about sepsis symptoms, treatment options, and prevention strategies to protect your health in the full article.
Table of Comparison
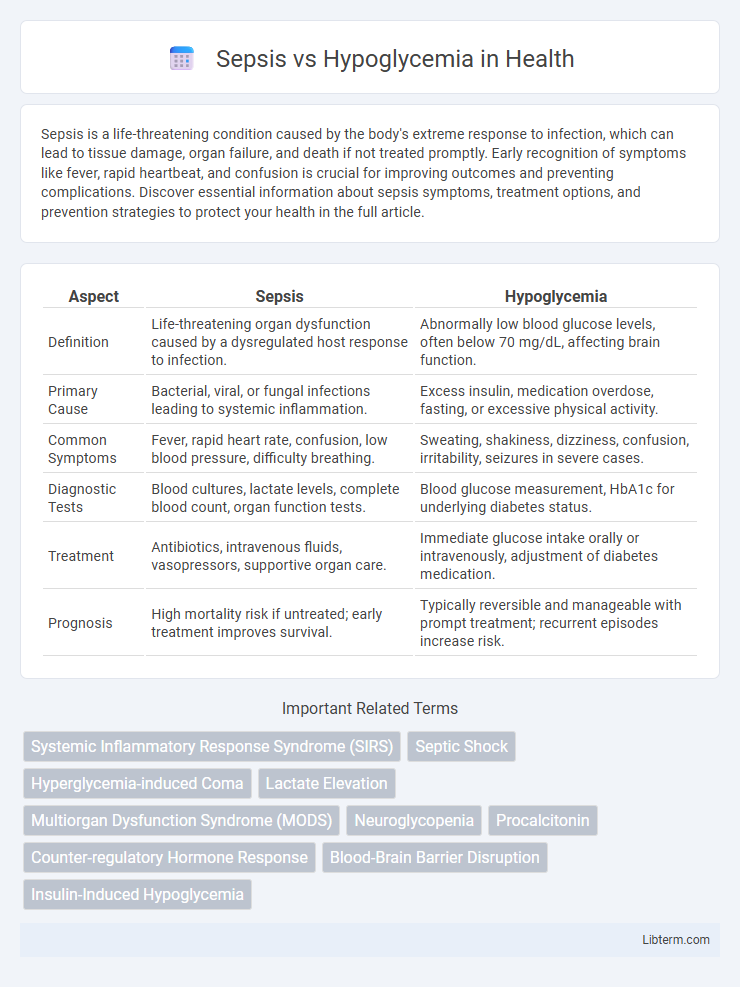
| Aspect | Sepsis | Hypoglycemia |
|---|---|---|
| Definition | Life-threatening organ dysfunction caused by a dysregulated host response to infection. | Abnormally low blood glucose levels, often below 70 mg/dL, affecting brain function. |
| Primary Cause | Bacterial, viral, or fungal infections leading to systemic inflammation. | Excess insulin, medication overdose, fasting, or excessive physical activity. |
| Common Symptoms | Fever, rapid heart rate, confusion, low blood pressure, difficulty breathing. | Sweating, shakiness, dizziness, confusion, irritability, seizures in severe cases. |
| Diagnostic Tests | Blood cultures, lactate levels, complete blood count, organ function tests. | Blood glucose measurement, HbA1c for underlying diabetes status. |
| Treatment | Antibiotics, intravenous fluids, vasopressors, supportive organ care. | Immediate glucose intake orally or intravenously, adjustment of diabetes medication. |
| Prognosis | High mortality risk if untreated; early treatment improves survival. | Typically reversible and manageable with prompt treatment; recurrent episodes increase risk. |
Understanding Sepsis: Definition and Causes
Sepsis is a life-threatening condition caused by the body's extreme response to infection, leading to tissue damage, organ failure, and potentially death. Common causes include bacterial infections in the lungs, urinary tract, skin, or gastrointestinal system that trigger widespread inflammation and systemic infection. Understanding sepsis requires recognizing its origins in infections and the body's dysregulated immune response, which is distinct from hypoglycemia's metabolic imbalance caused by low blood sugar levels.
Hypoglycemia Explained: What You Need to Know
Hypoglycemia occurs when blood glucose levels drop below 70 mg/dL, leading to symptoms like shakiness, confusion, and sweating. It requires prompt intervention with fast-acting carbohydrates and monitoring to prevent severe complications such as seizures or loss of consciousness. Differentiating hypoglycemia from sepsis is critical, as sepsis involves a systemic inflammatory response to infection with elevated heart rate, fever, and possible organ dysfunction, whereas hypoglycemia primarily affects metabolic and neurological functions.
Key Differences Between Sepsis and Hypoglycemia
Sepsis is a life-threatening systemic infection causing widespread inflammation and organ dysfunction, while hypoglycemia is characterized by abnormally low blood glucose levels primarily affecting brain function. Sepsis presents with fever, rapid heart rate, and hypotension, whereas hypoglycemia manifests as sweating, shakiness, confusion, and possible seizures due to neuroglycopenia. Diagnostic criteria for sepsis include confirmed infection and elevated inflammatory markers like procalcitonin, compared to blood glucose measurement below 70 mg/dL in hypoglycemia diagnosis.
Common Symptoms: Sepsis vs Hypoglycemia
Sepsis and hypoglycemia share several common symptoms, including confusion, sweating, and rapid heartbeat, which can complicate initial diagnosis. Both conditions may present with shivering or chills, but sepsis typically involves fever and signs of infection, whereas hypoglycemia often causes trembling and hunger. Prompt recognition of overlapping symptoms is critical for effective treatment and to prevent severe complications.
Risk Factors and Vulnerable Populations
Sepsis risk factors include advanced age, immunosuppression, chronic illnesses like diabetes and kidney disease, and recent surgery or hospitalization, predominantly affecting the elderly and critically ill. Hypoglycemia primarily endangers individuals with diabetes on insulin or sulfonylureas, those with kidney or liver dysfunction, and malnourished patients, particularly the elderly and children. Both conditions pose significant risks in hospital settings, requiring vigilant monitoring of vulnerable populations to prevent life-threatening complications.
Diagnostic Approaches: Sepsis and Hypoglycemia
Diagnostic approaches for sepsis involve blood cultures, lactate measurement, and inflammatory markers like C-reactive protein and procalcitonin to identify systemic infection and organ dysfunction. Hypoglycemia diagnosis primarily relies on measuring plasma glucose levels below 70 mg/dL alongside clinical symptoms such as sweating, confusion, and palpitations. Rapid bedside glucose testing complements laboratory assays, enabling timely differentiation between these critical conditions to guide appropriate treatment.
Emergency Management for Sepsis and Hypoglycemia
Emergency management of sepsis requires immediate administration of broad-spectrum intravenous antibiotics and aggressive fluid resuscitation to maintain hemodynamic stability and prevent organ dysfunction. In contrast, hypoglycemia treatment involves rapid correction of blood glucose levels through oral glucose intake or intravenous dextrose administration, depending on the patient's consciousness and severity of hypoglycemia. Continuous monitoring of vital signs and blood glucose levels is critical in both conditions to guide further therapeutic interventions and prevent complications.
Long-Term Complications and Prognosis
Sepsis often leads to long-term complications such as chronic organ dysfunction, cognitive impairment, and increased risk of relapse or secondary infections due to persistent inflammation and immune dysregulation. Hypoglycemia, particularly when recurrent or severe, can cause lasting neurological damage including memory loss, cognitive decline, and in extreme cases, seizures or coma. Prognosis for sepsis patients depends heavily on the severity and timeliness of treatment, whereas hypoglycemia outcomes improve significantly with prompt glucose replenishment but can worsen if episodes recur frequently or remain untreated.
Prevention Strategies for Sepsis and Hypoglycemia
Effective prevention strategies for sepsis include timely vaccination against influenza and pneumococcus, strict hygiene practices, early identification of infections, and prompt antibiotic treatment to reduce the risk of systemic infection. Hypoglycemia prevention centers on regular blood glucose monitoring, maintaining balanced meals rich in complex carbohydrates, and appropriate adjustment of insulin or oral hypoglycemic agents, especially in diabetic patients. Patient education on recognizing early symptoms and managing lifestyle factors plays a crucial role in minimizing the incidence of both sepsis and hypoglycemia.
When to Seek Immediate Medical Attention
Seek immediate medical attention for sepsis if symptoms include high fever, rapid heartbeat, confusion, severe shortness of breath, or persistent low blood pressure, as these indicate life-threatening infection requiring urgent treatment. For hypoglycemia, urgent care is needed when experiencing seizures, loss of consciousness, severe shakiness, or inability to swallow, since dangerously low blood sugar levels can cause brain damage without prompt intervention. Timely recognition and treatment of these critical signs can prevent irreversible complications and improve survival outcomes.
Sepsis Infographic
 libterm.com
libterm.com