Proper ventilation enhances indoor air quality by reducing pollutants, controlling humidity, and preventing mold growth, which contributes to a healthier living environment. Efficient ventilation systems also improve comfort and energy efficiency by regulating temperature and airflow. Discover how to optimize your ventilation setup for better air quality and energy savings in the rest of the article.
Table of Comparison
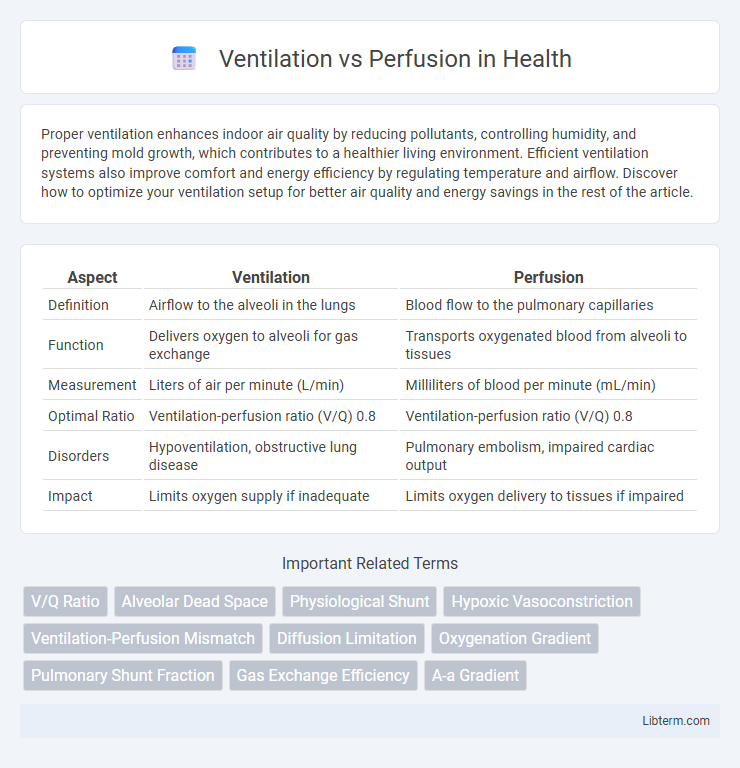
| Aspect | Ventilation | Perfusion |
|---|---|---|
| Definition | Airflow to the alveoli in the lungs | Blood flow to the pulmonary capillaries |
| Function | Delivers oxygen to alveoli for gas exchange | Transports oxygenated blood from alveoli to tissues |
| Measurement | Liters of air per minute (L/min) | Milliliters of blood per minute (mL/min) |
| Optimal Ratio | Ventilation-perfusion ratio (V/Q) 0.8 | Ventilation-perfusion ratio (V/Q) 0.8 |
| Disorders | Hypoventilation, obstructive lung disease | Pulmonary embolism, impaired cardiac output |
| Impact | Limits oxygen supply if inadequate | Limits oxygen delivery to tissues if impaired |
Understanding Ventilation and Perfusion
Ventilation refers to the process of moving air in and out of the lungs, delivering oxygen to the alveoli where gas exchange occurs. Perfusion is the flow of blood through pulmonary capillaries surrounding the alveoli, facilitating the uptake of oxygen and removal of carbon dioxide. Efficient respiratory function depends on the matching of ventilation and perfusion ratios to optimize oxygenation and maintain acid-base balance.
The Physiology of Gas Exchange
Ventilation refers to the movement of air into and out of the alveoli, ensuring oxygen reaches the lung's gas exchange surfaces. Perfusion involves the flow of blood through pulmonary capillaries, enabling the transport of oxygen and carbon dioxide between alveoli and bloodstream. Effective gas exchange depends on matching ventilation to perfusion (V/Q ratio) to optimize oxygen uptake and carbon dioxide removal.
Key Differences Between Ventilation and Perfusion
Ventilation refers to the process of air movement into and out of the lungs, enabling gas exchange to occur at the alveolar level, while perfusion is the flow of blood through pulmonary capillaries delivering oxygen to and removing carbon dioxide from tissues. The key difference lies in their functions: ventilation facilitates oxygen intake and carbon dioxide removal, whereas perfusion ensures blood circulation to transport gases throughout the body. Effective gas exchange requires a balanced ventilation-perfusion ratio, with any disproportion leading to impaired oxygenation or respiratory issues.
The V/Q Ratio Explained
The V/Q ratio represents the relationship between ventilation (airflow) and perfusion (blood flow) in the lungs, crucial for efficient gas exchange. A normal V/Q ratio is approximately 0.8, indicating that ventilation is slightly less than perfusion to optimize oxygen uptake and carbon dioxide removal. Imbalances such as V/Q mismatch can lead to respiratory conditions like hypoxemia, highlighting the importance of maintaining an ideal ventilation-perfusion balance.
Factors Affecting Ventilation
Ventilation is influenced by factors such as airway resistance, lung compliance, and respiratory muscle strength, which determine the volume and flow of air entering the alveoli. Airway resistance increases with bronchoconstriction or obstruction, reducing airflow, while decreased lung compliance impairs lung expansion and reduces ventilation efficiency. Proper ventilation is essential for effective gas exchange, as imbalances can disrupt oxygen delivery and carbon dioxide removal in the alveolar-capillary interface.
Factors Influencing Perfusion
Perfusion is influenced by cardiac output, blood volume, and vascular resistance, which determine the amount of blood reaching alveolar capillaries for gas exchange. Pulmonary vasoconstriction and factors such as hypoxia or embolism can reduce perfusion by limiting blood flow to certain lung regions. Gravity also plays a crucial role, causing perfusion to vary from the lung apex to the base, with increased blood flow in the lower lung zones due to hydrostatic pressure.
Common Ventilation-Perfusion Mismatches
Common ventilation-perfusion (V/Q) mismatches include shunt, dead space, and low V/Q ratio conditions. In shunt, perfusion occurs without ventilation, leading to hypoxemia and refractory hypoxia. Dead space represents ventilation without perfusion, causing inefficient gas exchange and increased work of breathing.
Clinical Implications of V/Q Imbalance
V/Q imbalance, defined as the mismatch between alveolar ventilation and pulmonary capillary perfusion, significantly impacts oxygenation and carbon dioxide elimination, often leading to hypoxemia. Clinical implications include conditions such as pulmonary embolism, where perfusion defects increase dead space ventilation, and chronic obstructive pulmonary disease (COPD), characterized by uneven ventilation causing shunting and impaired gas exchange. Understanding V/Q ratios through diagnostic tools like V/Q scanning and arterial blood gas analysis guides targeted treatment strategies, improving patient outcomes in respiratory and cardiovascular diseases.
Diagnostic Methods for Assessing V/Q
Diagnostic methods for assessing ventilation and perfusion include ventilation-perfusion (V/Q) scans, which use radioactive isotopes to visualize air and blood flow within the lungs. Pulmonary angiography offers detailed imaging of perfusion by injecting contrast material into the pulmonary arteries, while spirometry and arterial blood gas analysis provide indirect data on ventilation efficiency. Advanced imaging techniques like CT pulmonary angiography (CTPA) combine structural and functional assessment, enhancing the accuracy of V/Q mismatch diagnosis.
Strategies to Improve Ventilation-Perfusion Matching
Optimizing ventilation-perfusion matching involves adjusting ventilator settings to enhance alveolar ventilation while ensuring adequate pulmonary blood flow, reducing shunt and dead space effects. Strategies include using positive end-expiratory pressure (PEEP) to prevent alveolar collapse, prone positioning to redistribute ventilation and improve oxygenation, and targeted recruitment maneuvers to open collapsed lung units. Pharmacologic interventions like vasodilators can selectively improve perfusion to well-ventilated areas, promoting better gas exchange efficiency.
Ventilation Infographic
 libterm.com
libterm.com