Spinal anesthesia provides effective pain relief during surgeries by injecting anesthetic directly into the spinal fluid, ensuring targeted numbness and muscle relaxation. It is commonly used for lower body procedures, offering advantages such as rapid onset and minimal impact on overall consciousness. Explore the full article to understand how spinal anesthesia can benefit your surgical experience.
Table of Comparison
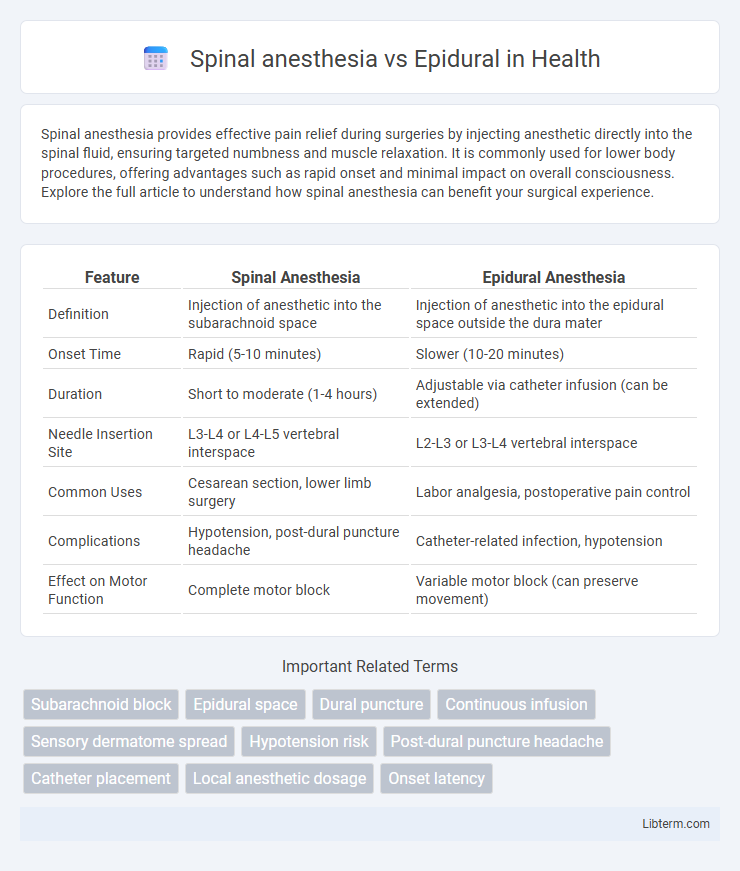
| Feature | Spinal Anesthesia | Epidural Anesthesia |
|---|---|---|
| Definition | Injection of anesthetic into the subarachnoid space | Injection of anesthetic into the epidural space outside the dura mater |
| Onset Time | Rapid (5-10 minutes) | Slower (10-20 minutes) |
| Duration | Short to moderate (1-4 hours) | Adjustable via catheter infusion (can be extended) |
| Needle Insertion Site | L3-L4 or L4-L5 vertebral interspace | L2-L3 or L3-L4 vertebral interspace |
| Common Uses | Cesarean section, lower limb surgery | Labor analgesia, postoperative pain control |
| Complications | Hypotension, post-dural puncture headache | Catheter-related infection, hypotension |
| Effect on Motor Function | Complete motor block | Variable motor block (can preserve movement) |
Introduction to Spinal and Epidural Anesthesia
Spinal anesthesia involves injecting local anesthetic into the subarachnoid space, producing a rapid and profound nerve block ideal for lower abdominal, pelvic, and lower limb surgeries. Epidural anesthesia requires the administration of anesthetic into the epidural space, allowing for gradual onset and adjustable sensory and motor blockade, commonly used in labor analgesia and extended postoperative pain control. Both techniques target nerve roots but differ in onset time, needle placement, and pharmacokinetics, influencing their clinical applications and safety profiles.
Key Differences Between Spinal and Epidural Techniques
Spinal anesthesia involves injecting a local anesthetic directly into the cerebrospinal fluid in the subarachnoid space, offering rapid and profound nerve blockade ideal for surgeries below the abdomen. Epidural anesthesia delivers the anesthetic into the epidural space outside the dura mater, allowing continuous infusion or intermittent dosing for adjustable and prolonged pain control, commonly used in labor and post-operative analgesia. Key differences include onset time, with spinal anesthesia acting within minutes, whereas epidural onset is slower, and the level of motor blockade, which is typically denser in spinal anesthesia compared to the more selective sensory blockade of epidurals.
Indications for Spinal vs Epidural Anesthesia
Spinal anesthesia is primarily indicated for surgeries involving the lower abdomen, pelvis, and lower extremities, offering rapid onset and dense motor and sensory blockade. Epidural anesthesia is preferred for longer-duration procedures, labor pain management, and postoperative analgesia due to its ability to provide continuous anesthesia with adjustable dosage. Patient conditions such as coagulopathy, infection at the injection site, and anatomical abnormalities influence the choice between spinal and epidural anesthesia to optimize safety and efficacy.
Procedure Steps: Spinal and Epidural Anesthesia
Spinal anesthesia involves a single injection of local anesthetic into the subarachnoid space, typically at the lumbar level, resulting in rapid onset and dense motor and sensory blockade. Epidural anesthesia requires catheter placement into the epidural space, allowing for continuous or intermittent delivery of anesthetic agents, providing adjustable and prolonged anesthesia. Both procedures use aseptic technique and patient positioning, but spinal anesthesia offers a simpler and faster approach, while epidural anesthesia offers greater flexibility in dosing and duration.
Duration and Onset of Anesthetic Effect
Spinal anesthesia typically has a rapid onset of action within 5 minutes and provides a dense, profound block that lasts approximately 1.5 to 4 hours depending on the local anesthetic used. Epidural anesthesia has a slower onset, usually taking 10 to 20 minutes to achieve adequate anesthetic effect, with durations that can extend from 1 to 3 hours and can be prolonged via catheter infusion. The choice between spinal and epidural anesthesia depends on the desired speed of onset and duration of effect required for surgical procedures or pain management.
Advantages of Spinal Anesthesia
Spinal anesthesia offers rapid onset and profound sensory and motor block with a single injection into the subarachnoid space, ensuring effective anesthesia for lower abdominal, pelvic, and lower limb surgeries. It requires a lower dose of local anesthetic compared to epidural anesthesia, reducing systemic toxicity risk and providing a denser block. This technique also allows for greater patient hemodynamic stability and a lower incidence of catheter-related complications.
Benefits of Epidural Anesthesia
Epidural anesthesia provides continuous pain relief during labor and surgery by administering medication through a catheter placed in the epidural space, allowing for dosage adjustments and prolonged control. It offers better pain management with fewer motor blockades compared to spinal anesthesia, enabling patients to remain more mobile. Epidurals also lower the risk of sudden hypotension and can be used for postoperative analgesia, enhancing overall comfort and recovery.
Risks and Complications Comparison
Spinal anesthesia carries risks such as hypotension, post-dural puncture headache, and rare but serious complications like spinal hematoma or infection, while epidural anesthesia poses potential complications including incomplete block, infection, epidural hematoma, and nerve damage. Both techniques carry the risk of neurological complications, though spinal anesthesia typically results in a faster onset and denser block, increasing the chance of hypotension. Epidurals offer more controlled anesthesia with adjustable dosage but require meticulous catheter placement to minimize risks of complications.
Patient Selection: Which Technique is Best?
Spinal anesthesia is often preferred for shorter, lower abdominal or lower extremity surgeries due to its rapid onset and profound sensory and motor blockade, making it ideal for patients with no contraindications like coagulopathy or infection at the injection site. Epidural anesthesia offers more controlled, adjustable dosing, beneficial for longer procedures or when postoperative pain control is desired, especially in patients with cardiac or respiratory comorbidities needing gradual hemodynamic changes. Careful patient selection depends on surgery duration, the need for postoperative analgesia, and underlying medical conditions to optimize safety and efficacy.
Conclusion: Choosing the Right Regional Anesthesia
Spinal anesthesia offers rapid onset and reliable anesthesia for lower body procedures, ideal for surgeries requiring dense sensory and motor block. Epidural anesthesia provides adjustable, prolonged pain control with the flexibility for catheter placement, making it suitable for longer surgeries and postoperative analgesia. Selecting between spinal and epidural anesthesia depends on factors such as procedure duration, patient condition, desired onset time, and the need for continuous pain management.
Spinal anesthesia Infographic
 libterm.com
libterm.com