Insulinoma is a rare pancreatic tumor that secretes excessive insulin, leading to hypoglycemia and symptoms such as dizziness, sweating, and confusion. Early diagnosis and treatment are crucial to prevent severe complications and improve quality of life. Discover essential insights about insulinoma, its symptoms, diagnosis, and treatment options in the rest of this article.
Table of Comparison
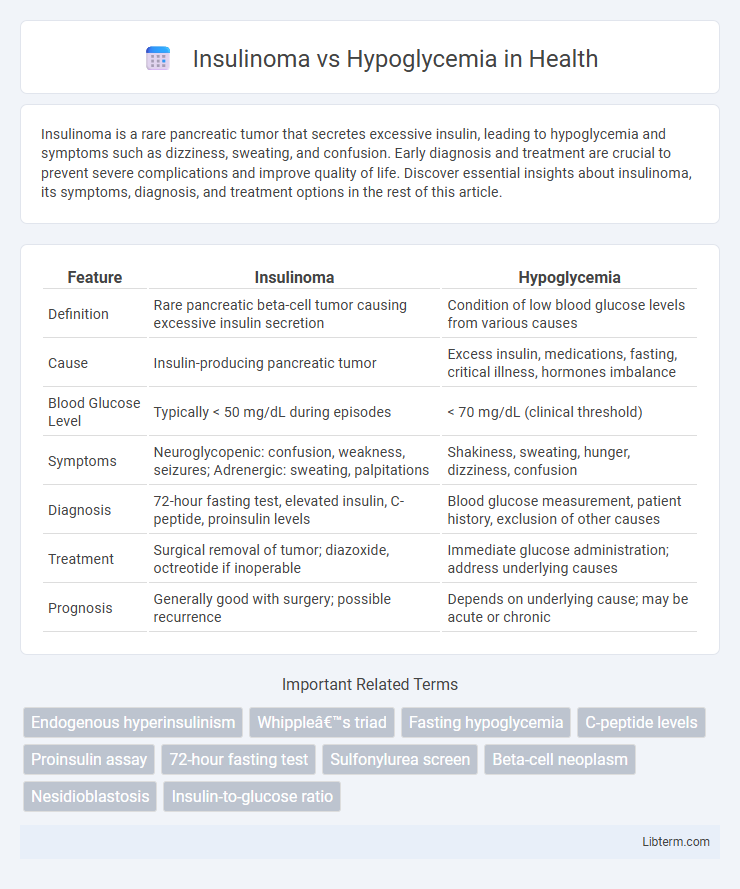
| Feature | Insulinoma | Hypoglycemia |
|---|---|---|
| Definition | Rare pancreatic beta-cell tumor causing excessive insulin secretion | Condition of low blood glucose levels from various causes |
| Cause | Insulin-producing pancreatic tumor | Excess insulin, medications, fasting, critical illness, hormones imbalance |
| Blood Glucose Level | Typically < 50 mg/dL during episodes | < 70 mg/dL (clinical threshold) |
| Symptoms | Neuroglycopenic: confusion, weakness, seizures; Adrenergic: sweating, palpitations | Shakiness, sweating, hunger, dizziness, confusion |
| Diagnosis | 72-hour fasting test, elevated insulin, C-peptide, proinsulin levels | Blood glucose measurement, patient history, exclusion of other causes |
| Treatment | Surgical removal of tumor; diazoxide, octreotide if inoperable | Immediate glucose administration; address underlying causes |
| Prognosis | Generally good with surgery; possible recurrence | Depends on underlying cause; may be acute or chronic |
Understanding Insulinoma and Hypoglycemia
Insulinoma is a rare pancreatic tumor that secretes excessive insulin, causing persistent hypoglycemia characterized by low blood sugar levels. Hypoglycemia occurs when blood glucose drops below normal, leading to symptoms like sweating, confusion, and dizziness, and can result from multiple causes including insulinoma, medication, or metabolic disorders. Diagnosing insulinoma involves measuring fasting insulin, C-peptide levels, and imaging studies, while hypoglycemia requires prompt blood sugar monitoring and treatment to prevent severe complications.
Causes and Pathophysiology
Insulinoma is a rare pancreatic beta-cell tumor that causes uncontrolled insulin secretion, leading to persistent hypoglycemia by increasing glucose uptake into tissues and inhibiting hepatic glucose production. Hypoglycemia can result from multiple causes, including excessive insulin administration, critical illnesses, hormone deficiencies, or metabolic disorders, each disrupting normal glucose homeostasis through different mechanisms. The pathophysiology of insulinoma involves autonomous insulin production independent of blood glucose levels, whereas hypoglycemia from other causes often arises from impaired glucose production, increased glucose utilization, or insulin excess.
Key Differences in Clinical Presentation
Insulinoma typically presents with recurrent episodes of fasting hypoglycemia characterized by neuroglycopenic symptoms such as confusion, sweating, and palpitations, whereas hypoglycemia from other causes often occurs postprandially or is associated with insulin therapy. Insulinoma-induced hypoglycemia shows inappropriately high insulin, C-peptide, and proinsulin levels during episodes, distinguishing it from exogenous insulin administration causing hypoglycemia where C-peptide is low. The diagnostic Whipple's triad--symptoms of hypoglycemia, low plasma glucose, and relief upon glucose administration--is more reliably observed in insulinoma compared to other hypoglycemic conditions.
Common Symptoms to Recognize
Insulinoma and hypoglycemia share overlapping common symptoms such as sweating, confusion, dizziness, and palpitations caused by low blood glucose levels. Insulinoma-induced hypoglycemia typically presents with recurrent episodes of neuroglycopenic symptoms, including blurred vision, weakness, and seizures, often relieved by food intake. Recognizing these symptoms alongside consistent low fasting glucose and elevated insulin levels helps differentiate insulinoma from other causes of hypoglycemia.
Diagnostic Approaches and Tests
Diagnosing insulinoma involves fasting tests, particularly a supervised 72-hour fast to detect inappropriately elevated insulin, C-peptide, and proinsulin levels despite hypoglycemia. Hypoglycemia diagnosis relies on Whipple's triad assessment, including symptoms of low blood glucose, measured plasma glucose under 55 mg/dL, and relief after glucose administration, supported by blood tests for insulin, C-peptide, and sulfonylurea levels to differentiate causes. Imaging studies such as endoscopic ultrasound, CT scan, or MRI help localize insulinomas, whereas hypoglycemia evaluation focuses on identifying underlying causes like medication effects or critical illness.
Laboratory Findings: Comparing Insulinoma and Hypoglycemia
Laboratory findings in insulinoma typically reveal inappropriately elevated insulin levels, increased C-peptide, and proinsulin during episodes of hypoglycemia, distinguishing it from other causes of hypoglycemia. In contrast, non-insulin-mediated hypoglycemia shows low insulin and C-peptide levels despite low blood glucose. Measurement of beta-hydroxybutyrate and sulfonylurea screens further aid in differentiating insulinoma from exogenous insulin use or other metabolic disorders.
Imaging Techniques for Localization
Imaging techniques for localization of insulinoma primarily include endoscopic ultrasound (EUS), which offers high sensitivity due to its proximity to the pancreas, and contrast-enhanced computed tomography (CT), providing detailed anatomical information and detection of small tumors. Magnetic resonance imaging (MRI) is also utilized, with its superior soft tissue contrast aiding in differentiating insulinomas from other pancreatic lesions. Functional imaging using positron emission tomography (PET) with tracers like 68Ga-DOTATATE can identify neuroendocrine tumors by targeting somatostatin receptors, enhancing localization accuracy in cases where conventional imaging is inconclusive.
Management and Treatment Options
Management of insulinoma involves surgical resection as the primary treatment to remove the insulin-secreting tumor, while medical therapy with diazoxide or octreotide is used to control hypoglycemia preoperatively or when surgery is not feasible. Hypoglycemia without insulinoma requires addressing the underlying cause, such as adjusting diabetes medications or providing glucose supplementation in cases of reactive or fasting hypoglycemia. Continuous glucose monitoring and dietary modifications with frequent small meals are essential strategies to prevent recurrent hypoglycemic episodes in both conditions.
Prognosis and Long-term Outcomes
Insulinoma, a rare pancreatic neuroendocrine tumor causing endogenous hyperinsulinemic hypoglycemia, generally has a favorable prognosis after surgical resection, with most patients experiencing symptom resolution and a high 5-year survival rate above 90%. In contrast, hypoglycemia without insulinoma, often due to other metabolic or endocrine disorders, may have variable outcomes depending on the underlying cause and management effectiveness, with recurrent episodes potentially leading to neurological damage or cognitive decline over time. Long-term outcomes for insulinoma patients are generally positive if diagnosed early, while non-tumor hypoglycemia requires tailored treatment to prevent complications and improve quality of life.
When to Seek Medical Attention
Seek medical attention immediately if symptoms such as persistent low blood sugar, confusion, sweating, or fainting occur, as these may indicate an insulinoma or severe hypoglycemia. Rapid glucose testing and professional evaluation are critical to differentiate between insulinoma, a rare pancreatic tumor causing excess insulin, and other causes of hypoglycemia. Early diagnosis and treatment prevent complications like seizures, loss of consciousness, and potential brain damage.
Insulinoma Infographic
 libterm.com
libterm.com