Mastitis and inflammatory breast cancer both cause redness, swelling, and pain in the breast, but their treatment and outcomes differ dramatically. While mastitis is typically an infection treated with antibiotics, inflammatory breast cancer requires prompt medical intervention due to its aggressive nature. Learn how to distinguish between these conditions and protect your breast health by reading the full article.
Table of Comparison
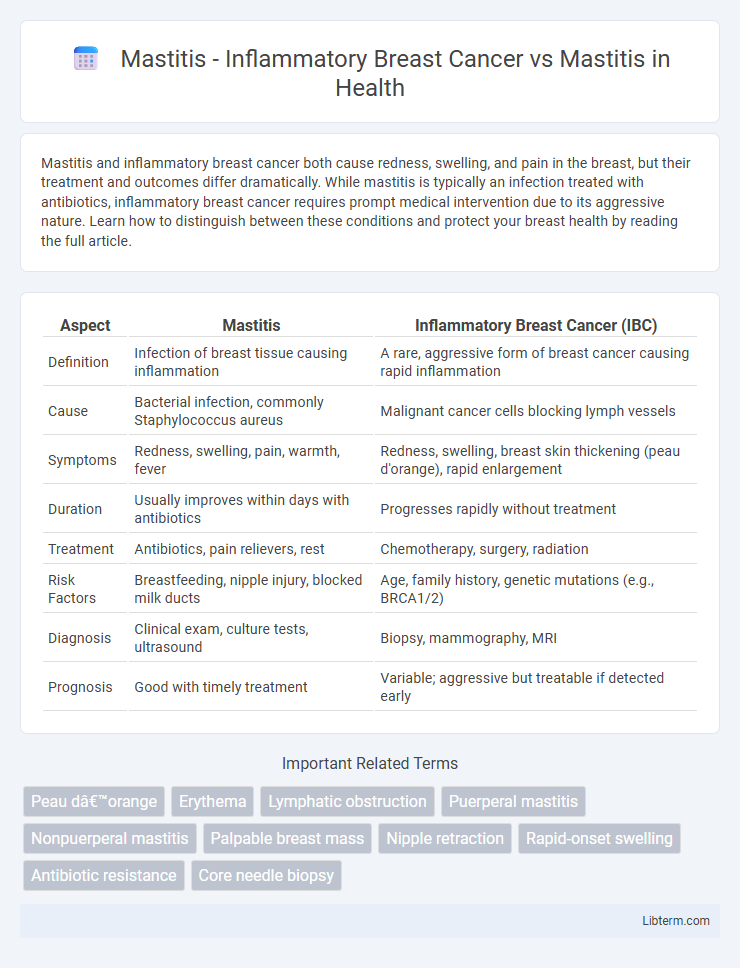
| Aspect | Mastitis | Inflammatory Breast Cancer (IBC) |
|---|---|---|
| Definition | Infection of breast tissue causing inflammation | A rare, aggressive form of breast cancer causing rapid inflammation |
| Cause | Bacterial infection, commonly Staphylococcus aureus | Malignant cancer cells blocking lymph vessels |
| Symptoms | Redness, swelling, pain, warmth, fever | Redness, swelling, breast skin thickening (peau d'orange), rapid enlargement |
| Duration | Usually improves within days with antibiotics | Progresses rapidly without treatment |
| Treatment | Antibiotics, pain relievers, rest | Chemotherapy, surgery, radiation |
| Risk Factors | Breastfeeding, nipple injury, blocked milk ducts | Age, family history, genetic mutations (e.g., BRCA1/2) |
| Diagnosis | Clinical exam, culture tests, ultrasound | Biopsy, mammography, MRI |
| Prognosis | Good with timely treatment | Variable; aggressive but treatable if detected early |
Understanding Mastitis: Causes and Symptoms
Mastitis primarily stems from bacterial infection or milk stasis, leading to inflammation and redness in the breast tissue, accompanied by pain, swelling, and fever. Inflammatory Breast Cancer (IBC), although sharing symptoms like swelling and redness, reveals a rapidly progressing condition with skin changes such as peau d'orange and nipple retraction, distinguishing it from typical mastitis. Accurate diagnosis requires clinical evaluation and imaging to differentiate bacterial mastitis from aggressive cancers to ensure prompt and appropriate treatment.
What is Inflammatory Breast Cancer?
Inflammatory Breast Cancer (IBC) is a rare and aggressive form of breast cancer characterized by rapid onset of redness, swelling, and warmth in the breast, often without a distinct lump. Unlike mastitis, which is a benign infection of the breast tissue predominantly affecting breastfeeding women and responsive to antibiotics, IBC involves cancer cells blocking lymphatic vessels, leading to skin changes resembling inflammation. Early diagnosis and treatment are critical, as IBC progresses quickly and requires a combination of chemotherapy, surgery, and radiation.
Differentiating Mastitis from Inflammatory Breast Cancer
Differentiating mastitis from inflammatory breast cancer (IBC) is crucial as both conditions present with breast inflammation, redness, and swelling but require distinct treatments. Mastitis, typically caused by bacterial infection during lactation, responds well to antibiotics and usually resolves within days, whereas IBC is an aggressive malignancy characterized by rapid onset, peau d'orange skin changes, and often no distinct lump. Diagnostic imaging such as mammography, ultrasound, and biopsy are essential to distinguish IBC from mastitis, especially when symptoms persist or worsen despite standard antibiotic therapy.
Risk Factors for Mastitis and Inflammatory Breast Cancer
Mastitis primarily affects breastfeeding women due to nipple damage or milk stasis, with bacterial infection from Staphylococcus aureus being a common risk factor. Inflammatory breast cancer (IBC), a rare and aggressive cancer subtype, is linked to risk factors such as advanced age, African American ethnicity, obesity, and a history of breast cancer or atypical hyperplasia. While mastitis involves acute inflammation often resolving with antibiotics, IBC manifests rapidly with skin changes and requires immediate oncological evaluation due to its distinct pathophysiology and poor prognosis.
Key Symptoms: Mastitis vs Inflammatory Breast Cancer
Mastitis typically presents with localized breast pain, swelling, redness, warmth, and fever, often linked to breastfeeding or infection. Inflammatory Breast Cancer (IBC) exhibits similar symptoms but includes rapid onset of skin thickening, dimpling (peau d'orange), and persistent breast enlargement without infection signs. Differentiating key symptoms involves recognizing that IBC symptoms worsen quickly and do not improve with antibiotics, necessitating urgent medical evaluation.
Diagnostic Approaches for Breast Inflammation
Diagnostic approaches for distinguishing inflammatory breast cancer (IBC) from mastitis involve clinical evaluation, imaging, and biopsy. Mammography and ultrasound identify skin thickening, masses, and lymph node involvement but are insufficient alone for differentiation. A definitive diagnosis requires skin punch biopsy or core needle biopsy to detect malignant cells indicative of IBC, while mastitis typically shows infection-related inflammation without cancerous pathology.
Treatment Strategies: Mastitis vs Inflammatory Breast Cancer
Mastitis treatment primarily involves antibiotics targeting bacterial infection and supportive care, such as warm compresses and pain management, to reduce inflammation and promote healing. Inflammatory breast cancer (IBC) requires aggressive multimodal therapy, including systemic chemotherapy, surgery (usually mastectomy), and radiation therapy, reflecting its rapid progression and poor prognosis compared to mastitis. Accurate diagnosis through biopsy and imaging is critical, as IBC presents similarly to mastitis but necessitates an entirely different treatment approach focused on oncologic control rather than infection resolution.
When to Seek Medical Attention
Persistent breast redness, swelling, and pain lasting more than a week or worsening despite antibiotic treatment may indicate inflammatory breast cancer rather than typical mastitis. Seek immediate medical attention if symptoms include rapid breast enlargement, skin dimpling, nipple retraction, or unexplained weight loss, as these are signs of a more serious condition. Early diagnosis through a biopsy and imaging studies is crucial for effective treatment and improved outcomes.
Preventing Misdiagnosis: Red Flags to Watch For
Mastitis and Inflammatory Breast Cancer (IBC) share similar symptoms such as breast redness, swelling, and pain, which often leads to misdiagnosis. Red flags to watch for include lack of response to antibiotics within two weeks, presence of a palpable breast lump, skin dimpling, and nipple retraction, signaling the need for immediate further diagnostic testing like a biopsy or imaging. Early recognition of these warning signs is crucial to differentiate IBC from mastitis and ensure timely and appropriate treatment.
Support and Recovery: Patient Resources and Next Steps
Support and recovery for inflammatory breast cancer (IBC) and mastitis differ significantly due to the severity and treatment complexity of each condition. Patient resources for mastitis primarily focus on infection management and pain relief through antibiotics and lactation support, promoting quick recovery and breastfeeding continuation. In contrast, IBC requires comprehensive oncology support, including specialized cancer care teams, targeted therapies, and psychological counseling, with next steps emphasizing early diagnosis, aggressive treatment, and long-term follow-up to improve prognosis and quality of life.
Mastitis - Inflammatory Breast Cancer Infographic
 libterm.com
libterm.com