Lupus, also known as Systemic Lupus Erythematosus, is a chronic autoimmune disease where the immune system mistakenly attacks healthy tissues, causing inflammation and damage to multiple organs. Symptoms can vary widely, affecting the skin, joints, kidneys, and other parts of the body, making early diagnosis and tailored treatment essential for managing the condition. Explore the rest of the article to learn more about lupus symptoms, causes, and treatment options to better understand how it may impact your health.
Table of Comparison
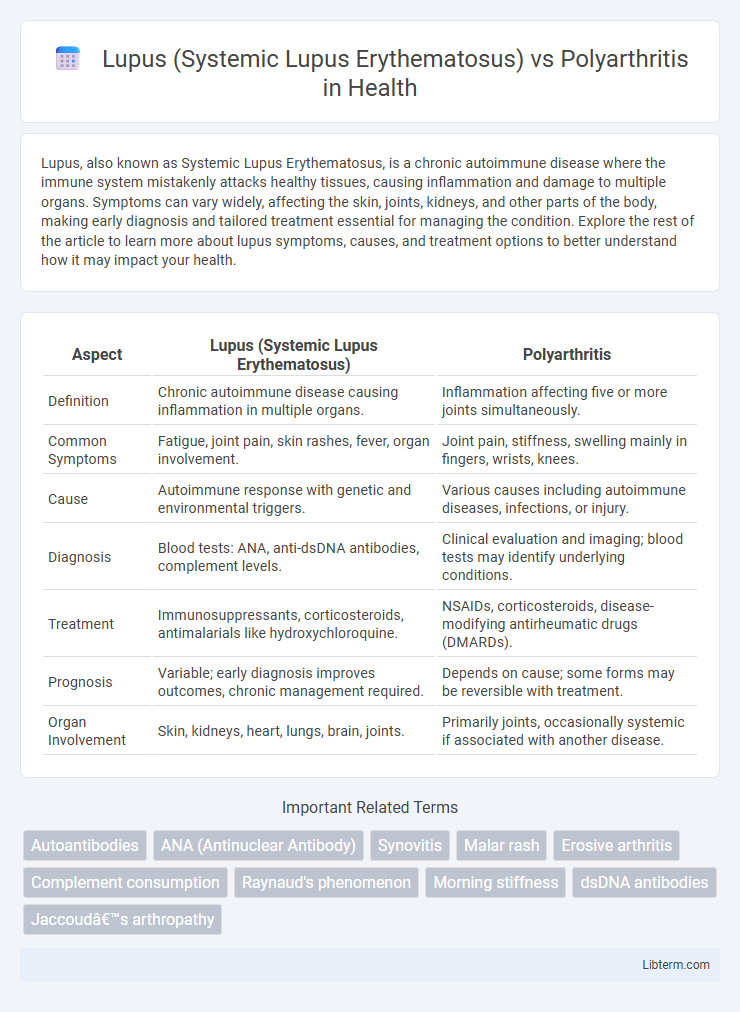
| Aspect | Lupus (Systemic Lupus Erythematosus) | Polyarthritis |
|---|---|---|
| Definition | Chronic autoimmune disease causing inflammation in multiple organs. | Inflammation affecting five or more joints simultaneously. |
| Common Symptoms | Fatigue, joint pain, skin rashes, fever, organ involvement. | Joint pain, stiffness, swelling mainly in fingers, wrists, knees. |
| Cause | Autoimmune response with genetic and environmental triggers. | Various causes including autoimmune diseases, infections, or injury. |
| Diagnosis | Blood tests: ANA, anti-dsDNA antibodies, complement levels. | Clinical evaluation and imaging; blood tests may identify underlying conditions. |
| Treatment | Immunosuppressants, corticosteroids, antimalarials like hydroxychloroquine. | NSAIDs, corticosteroids, disease-modifying antirheumatic drugs (DMARDs). |
| Prognosis | Variable; early diagnosis improves outcomes, chronic management required. | Depends on cause; some forms may be reversible with treatment. |
| Organ Involvement | Skin, kidneys, heart, lungs, brain, joints. | Primarily joints, occasionally systemic if associated with another disease. |
Understanding Systemic Lupus Erythematosus (SLE)
Systemic Lupus Erythematosus (SLE) is a chronic autoimmune disease characterized by widespread inflammation affecting multiple organs, including the skin, joints, kidneys, and nervous system. Unlike polyarthritis, which primarily involves joint inflammation, SLE presents with diverse symptoms such as fatigue, fever, malar rash, and renal involvement, making diagnosis complex. Autoantibody production, particularly antinuclear antibodies (ANA), plays a crucial role in SLE pathogenesis, distinguishing it from other rheumatic diseases.
What is Polyarthritis?
Polyarthritis is an inflammatory condition characterized by the simultaneous inflammation of five or more joints, leading to pain, swelling, and stiffness. Unlike Systemic Lupus Erythematosus (SLE), which is an autoimmune disease affecting multiple organ systems including joints, polyarthritis specifically targets joint inflammation without systemic organ involvement. Common causes of polyarthritis include rheumatoid arthritis, viral infections, and other autoimmune diseases, highlighting its role as a symptom rather than a standalone diagnosis.
Key Differences Between SLE and Polyarthritis
Systemic Lupus Erythematosus (SLE) is an autoimmune disease characterized by multi-organ involvement including skin, kidneys, and central nervous system, while polyarthritis primarily refers to inflammation affecting five or more joints. SLE presents with diverse symptoms such as malar rash, photosensitivity, and positive antinuclear antibodies (ANA), whereas polyarthritis often shows joint swelling, stiffness, and rheumatoid factor or anti-CCP antibodies when linked to conditions like rheumatoid arthritis. Unlike polyarthritis which predominantly affects joints, SLE can cause systemic complications like lupus nephritis and hematologic abnormalities, underscoring its broader clinical impact.
Common Symptoms: SLE vs Polyarthritis
Systemic Lupus Erythematosus (SLE) and polyarthritis both present with joint pain and swelling, but SLE symptoms are often accompanied by fatigue, fever, and a characteristic malar rash. Polyarthritis primarily involves inflammation and stiffness in multiple joints, commonly affecting the hands, wrists, and knees without the systemic manifestations seen in SLE. While both conditions cause joint discomfort, SLE's autoimmune nature leads to widespread symptoms beyond the joints, distinguishing it from polyarthritis.
Causes and Risk Factors
Systemic Lupus Erythematosus (SLE) is an autoimmune disease triggered by a combination of genetic predisposition, environmental factors such as UV light exposure, infections, and hormone imbalances, predominantly affecting women of childbearing age. Polyarthritis often results from autoimmune conditions like rheumatoid arthritis or infectious causes, with risk factors including family history, smoking, and certain viral or bacterial infections. Both conditions share immune system dysregulation but differ in specific triggers and the spectrum of genetic and environmental contributions.
Diagnosis: Tests and Procedures
Diagnosis of Systemic Lupus Erythematosus (SLE) involves antinuclear antibody (ANA) testing, anti-double stranded DNA (anti-dsDNA), and anti-Smith antibodies, along with complete blood count (CBC) and urinalysis to assess organ involvement. Polyarthritis diagnosis includes rheumatoid factor (RF), anti-cyclic citrullinated peptide (anti-CCP) antibodies, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) to evaluate inflammation and joint damage. Imaging studies such as X-rays and ultrasound assist in distinguishing joint erosion patterns characteristic of polyarthritis from soft tissue disease in lupus.
Treatment Options for SLE
Systemic Lupus Erythematosus (SLE) treatment primarily involves immunosuppressive medications such as corticosteroids, antimalarials like hydroxychloroquine, and biologics like belimumab to reduce inflammation and prevent organ damage. Management of polyarthritis, particularly when associated with rheumatoid arthritis, often includes disease-modifying antirheumatic drugs (DMARDs) such as methotrexate and nonsteroidal anti-inflammatory drugs (NSAIDs) to control joint symptoms. Tailoring therapy for SLE focuses on controlling systemic autoimmune activity, contrasting with polyarthritis treatments that target synovial inflammation and joint preservation.
Treatment Approaches for Polyarthritis
Treatment approaches for polyarthritis primarily involve the use of disease-modifying antirheumatic drugs (DMARDs) such as methotrexate, which helps to reduce joint inflammation and prevent further damage. Nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids may be prescribed to manage pain and acute flare-ups. Physical therapy and lifestyle modifications also play crucial roles in maintaining joint function and improving quality of life for polyarthritis patients.
Living with Chronic Joint Conditions
Living with chronic joint conditions like Systemic Lupus Erythematosus (SLE) and polyarthritis requires comprehensive management of symptoms such as joint pain, swelling, and stiffness. SLE, an autoimmune disease, often affects multiple organs alongside joints, demanding tailored immunosuppressive therapies and lifestyle adjustments to reduce flares. In polyarthritis, characterized by inflammation in multiple joints often related to rheumatoid arthritis or other causes, sustained physical therapy, pain management, and disease-modifying antirheumatic drugs (DMARDs) play critical roles in maintaining mobility and quality of life.
Prognosis and Long-Term Management
Systemic Lupus Erythematosus (SLE) prognosis varies widely, with potential organ damage requiring vigilant long-term management using immunosuppressants and regular monitoring to prevent flares. Polyarthritis prognosis depends on the underlying cause but often involves chronic joint inflammation managed through disease-modifying antirheumatic drugs (DMARDs) and lifestyle modifications to preserve joint function. Both conditions demand tailored treatment plans emphasizing early intervention, symptom control, and ongoing patient education to improve quality of life and reduce complications.
Lupus (Systemic Lupus Erythematosus) Infographic
 libterm.com
libterm.com