Pulmonary embolism occurs when a blood clot blocks arteries in the lungs, causing sudden chest pain, shortness of breath, and potentially life-threatening complications. Early diagnosis and treatment are critical to prevent serious damage to lung tissue and improve survival rates. Discover how to recognize symptoms, understand risk factors, and explore treatment options in the rest of the article.
Table of Comparison
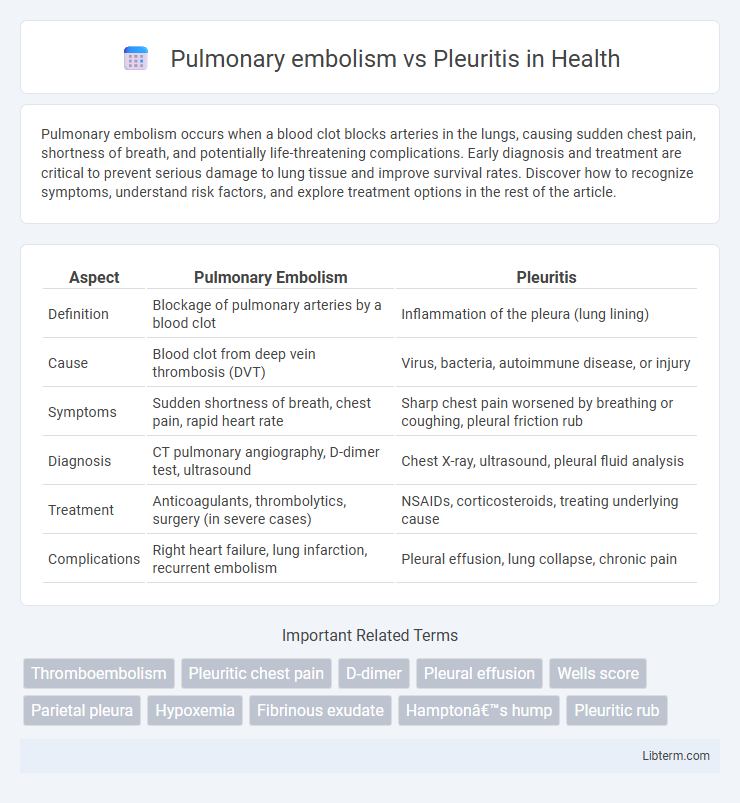
| Aspect | Pulmonary Embolism | Pleuritis |
|---|---|---|
| Definition | Blockage of pulmonary arteries by a blood clot | Inflammation of the pleura (lung lining) |
| Cause | Blood clot from deep vein thrombosis (DVT) | Virus, bacteria, autoimmune disease, or injury |
| Symptoms | Sudden shortness of breath, chest pain, rapid heart rate | Sharp chest pain worsened by breathing or coughing, pleural friction rub |
| Diagnosis | CT pulmonary angiography, D-dimer test, ultrasound | Chest X-ray, ultrasound, pleural fluid analysis |
| Treatment | Anticoagulants, thrombolytics, surgery (in severe cases) | NSAIDs, corticosteroids, treating underlying cause |
| Complications | Right heart failure, lung infarction, recurrent embolism | Pleural effusion, lung collapse, chronic pain |
Introduction to Pulmonary Embolism and Pleuritis
Pulmonary embolism (PE) is a life-threatening condition characterized by the sudden blockage of pulmonary arteries, typically caused by blood clots originating from deep vein thrombosis. Pleuritis, or pleurisy, involves inflammation of the pleura, the membrane surrounding the lungs, often resulting from infections or autoimmune diseases. Differentiating PE from pleuritis is critical due to their overlapping symptoms such as chest pain and shortness of breath but requires distinct diagnostic approaches and treatments based on underlying pathophysiology.
Defining Pulmonary Embolism
Pulmonary embolism is a life-threatening condition caused by the obstruction of the pulmonary arteries, usually due to a blood clot originating from deep vein thrombosis in the legs. This blockage disrupts blood flow to lung tissue, resulting in symptoms like sudden shortness of breath, chest pain, and coughing up blood. In contrast, pleuritis, or pleurisy, is inflammation of the pleura--the membrane surrounding the lungs--typically causing sharp chest pain that worsens with breathing but does not involve blood flow obstruction.
Defining Pleuritis
Pleuritis, also known as pleurisy, is an inflammation of the pleura, the thin membranes lining the lungs and chest cavity, causing sharp chest pain that worsens with breathing or coughing. This condition contrasts with pulmonary embolism, which involves a blockage of pulmonary arteries due to blood clots, leading to sudden shortness of breath, chest pain, and potential life-threatening complications. Accurate differentiation between pleuritis and pulmonary embolism is critical for effective treatment, often involving imaging studies like chest X-rays or CT scans and evaluation of clinical symptoms.
Causes and Risk Factors: Pulmonary Embolism vs Pleuritis
Pulmonary embolism primarily results from deep vein thrombosis, with risk factors including prolonged immobility, recent surgery, cancer, and inherited blood clotting disorders. Pleuritis, or pleurisy, is caused by inflammation of the pleura due to infections such as pneumonia or tuberculosis, autoimmune diseases like lupus, and chest trauma. While pulmonary embolism involves vascular obstruction, pleuritis stems from inflammatory processes affecting the pleural layers.
Key Symptoms: Comparison and Contrast
Pulmonary embolism typically presents with sudden onset dyspnea, pleuritic chest pain, tachycardia, and sometimes hemoptysis, reflecting obstruction of pulmonary arteries and impaired gas exchange. Pleuritis, or pleurisy, primarily causes sharp, localized chest pain worsening with deep breaths or coughing, often accompanied by friction rub without systemic symptoms like tachycardia or hypoxia. While both conditions involve pleuritic chest pain, pulmonary embolism frequently manifests systemic signs and respiratory distress, distinguishing it from the more localized inflammatory symptoms of pleuritis.
Diagnostic Approaches for Both Conditions
Pulmonary embolism diagnosis relies primarily on imaging techniques such as computed tomography pulmonary angiography (CTPA) and ventilation-perfusion (V/Q) scans, combined with D-dimer blood tests to assess clot presence. In contrast, pleuritis diagnosis frequently involves chest X-rays and ultrasound to detect pleural effusions, with pleural fluid analysis and thoracentesis used to identify inflammation or infection. Both conditions may require arterial blood gas analysis and electrocardiogram (ECG) to evaluate oxygenation and rule out cardiac causes of chest pain.
Treatment Options: Pulmonary Embolism vs Pleuritis
Pulmonary embolism treatment primarily involves anticoagulant medications such as heparin and warfarin to prevent clot progression, with thrombolytic therapy or surgical embolectomy reserved for severe cases. Pleuritis treatment centers on addressing the underlying cause, employing NSAIDs or corticosteroids to reduce pleural inflammation and pain, alongside antibiotics if infection is present. Effective management of pulmonary embolism requires rapid intervention due to the risk of mortality, whereas pleuritis treatment focuses on symptom relief and resolving inflammation.
Potential Complications and Prognosis
Pulmonary embolism can lead to life-threatening complications such as right ventricular dysfunction, pulmonary infarction, and chronic thromboembolic pulmonary hypertension, with prognosis heavily dependent on the size and location of the embolus. Pleuritis, if untreated or recurrent, may cause pleural effusions or fibrothorax, typically resulting in a favorable prognosis once the underlying cause is addressed. Early diagnosis and appropriate management significantly improve outcomes for both conditions.
Prevention Strategies for Both Conditions
Prevention of pulmonary embolism involves anticoagulant therapy, early mobilization after surgery, and use of compression stockings to reduce deep vein thrombosis risk. For pleuritis, prevention centers on treating underlying infections promptly and avoiding respiratory irritants like smoking and pollutants. Both conditions benefit from maintaining cardiovascular and respiratory health through regular exercise and vaccination against respiratory infections.
When to Seek Medical Attention
Seek medical attention immediately if experiencing sudden shortness of breath, chest pain that worsens with deep breathing, or rapid heartbeat, as these symptoms may indicate a pulmonary embolism requiring urgent intervention. For pleuritis, persistent sharp chest pain that intensifies during breathing, coughing, or movement alongside fever and difficulty breathing warrants prompt medical evaluation. Early diagnosis and treatment are critical for both conditions to prevent complications such as respiratory failure or circulatory collapse.
Pulmonary embolism Infographic
 libterm.com
libterm.com