Glomerulonephritis is an inflammatory condition affecting the kidney's filtering units called glomeruli, leading to impaired kidney function and potential progression to chronic kidney disease. Symptoms may include hematuria, proteinuria, hypertension, and edema, requiring timely diagnosis and management to prevent complications. Explore the full article to understand the causes, symptoms, treatment options, and how you can protect your kidney health.
Table of Comparison
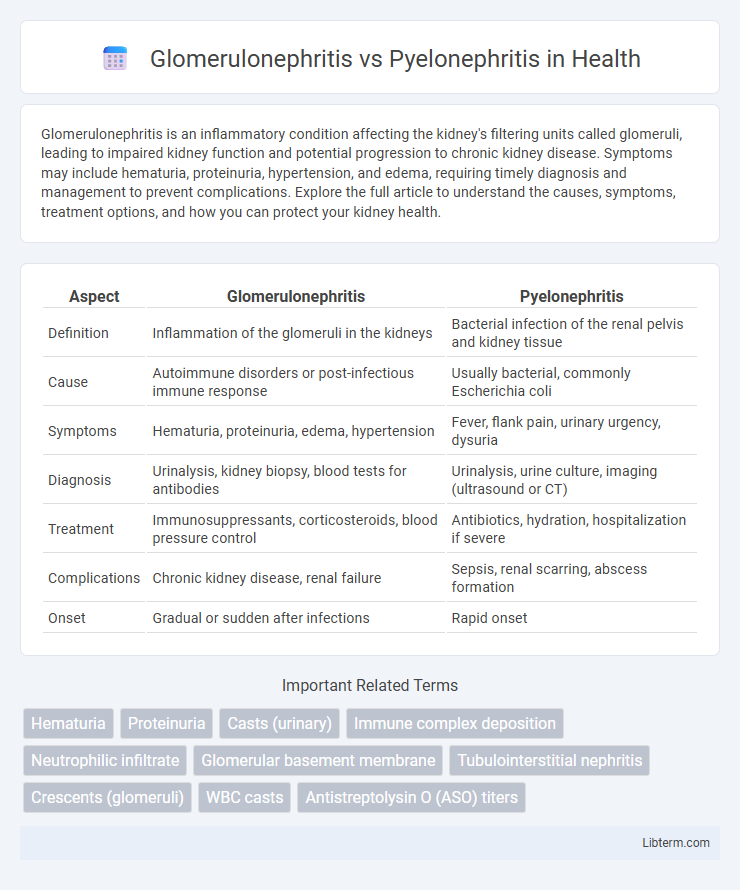
| Aspect | Glomerulonephritis | Pyelonephritis |
|---|---|---|
| Definition | Inflammation of the glomeruli in the kidneys | Bacterial infection of the renal pelvis and kidney tissue |
| Cause | Autoimmune disorders or post-infectious immune response | Usually bacterial, commonly Escherichia coli |
| Symptoms | Hematuria, proteinuria, edema, hypertension | Fever, flank pain, urinary urgency, dysuria |
| Diagnosis | Urinalysis, kidney biopsy, blood tests for antibodies | Urinalysis, urine culture, imaging (ultrasound or CT) |
| Treatment | Immunosuppressants, corticosteroids, blood pressure control | Antibiotics, hydration, hospitalization if severe |
| Complications | Chronic kidney disease, renal failure | Sepsis, renal scarring, abscess formation |
| Onset | Gradual or sudden after infections | Rapid onset |
Introduction to Glomerulonephritis and Pyelonephritis
Glomerulonephritis is an inflammation of the glomeruli, the kidney's tiny filtering units, often caused by immune responses or infections, leading to impaired kidney function and proteinuria. Pyelonephritis is a bacterial infection of the kidney's renal pelvis and interstitium, usually resulting from a lower urinary tract infection ascending into the kidneys. Both conditions affect renal health but differ in their pathophysiology, typical symptoms, and treatment approaches.
Definition and Overview
Glomerulonephritis is an inflammation of the glomeruli, the tiny filtering units within the kidneys responsible for blood filtration. Pyelonephritis refers to a bacterial infection of the renal pelvis and kidney tissue, commonly caused by ascending urinary tract infections. Both conditions impair kidney function but differ in etiology, pathology, and clinical management.
Causes and Risk Factors
Glomerulonephritis is primarily caused by autoimmune diseases such as lupus or post-streptococcal infections leading to inflammation of the kidney's glomeruli, with risk factors including a history of infections or genetic predisposition. Pyelonephritis results from bacterial infection, typically Escherichia coli, ascending from the lower urinary tract to the kidneys, with major risk factors including urinary tract obstruction, vesicoureteral reflux, and impaired immune function. Both conditions involve kidney inflammation but differ markedly in their etiology and predisposing factors.
Pathophysiology: Key Differences
Glomerulonephritis primarily involves immune-mediated inflammation of the glomeruli, often triggered by infections or autoimmune diseases, leading to impaired filtration and proteinuria. Pyelonephritis is characterized by bacterial infection that ascends from the lower urinary tract to the renal pelvis and interstitium, causing acute inflammation and potential abscess formation. Immune complex deposition drives glomerular injury in glomerulonephritis, whereas pyelonephritis results from direct bacterial invasion and neutrophil response in the renal parenchyma.
Clinical Presentation and Symptoms
Glomerulonephritis commonly presents with hematuria, proteinuria, edema, and hypertension, reflecting inflammation of the glomeruli and impaired kidney filtration. Pyelonephritis typically manifests with fever, flank pain, dysuria, and urinary frequency, indicating a bacterial infection of the renal pelvis and kidney parenchyma. Differentiating these conditions relies on clinical symptoms combined with laboratory findings such as elevated serum creatinine in glomerulonephritis and positive urine cultures in pyelonephritis.
Diagnostic Approaches
Glomerulonephritis diagnosis primarily involves urinalysis revealing hematuria, proteinuria, and red blood cell casts, along with serologic tests such as anti-streptolysin O titers and complement levels (C3, C4) to identify immune-mediated causes. Pyelonephritis is typically diagnosed through clinical symptoms like flank pain and fever, confirmed by urine culture showing significant bacteriuria, and imaging studies such as ultrasound or CT scan to detect renal inflammation or abscess. Differentiating between these conditions relies on combining laboratory markers of glomerular injury with microbiological and radiological evidence of upper urinary tract infection.
Laboratory and Imaging Findings
Glomerulonephritis presents with laboratory findings of hematuria, red blood cell casts, proteinuria, and elevated serum creatinine, often accompanied by decreased complement levels, especially C3, suggesting immune complex involvement. Imaging studies like renal ultrasound typically show normal-sized or slightly enlarged kidneys without signs of obstruction, as the pathology is intrinsic to the glomeruli. In contrast, pyelonephritis is characterized by pyuria, bacteriuria, and elevated white blood cell count in laboratory tests, with renal ultrasound revealing unilateral or bilateral renal enlargement, possible renal abscesses, or areas of hypoechogenicity indicating infection in the renal parenchyma.
Treatment Strategies
Treatment strategies for Glomerulonephritis primarily involve immunosuppressive therapies such as corticosteroids and cytotoxic drugs to reduce inflammation and prevent further kidney damage. Pyelonephritis requires prompt, targeted antibiotic therapy based on the causative bacterial pathogen, often involving fluoroquinolones or trimethoprim-sulfamethoxazole to resolve infection. Supportive care, including hydration and pain management, is crucial for both conditions to improve patient outcomes.
Complications and Prognosis
Glomerulonephritis complications include chronic kidney disease, nephrotic syndrome, and hypertension, often leading to end-stage renal disease if untreated. Pyelonephritis complications involve renal abscess, sepsis, and permanent kidney scarring, with prognosis generally favorable when promptly treated. Early diagnosis and targeted antibiotic therapy improve outcomes in pyelonephritis, while glomerulonephritis prognosis depends on underlying cause and response to immunosuppressive treatment.
Prevention and Patient Education
Preventing glomerulonephritis involves managing underlying conditions such as hypertension and autoimmune diseases through regular medical check-ups and adherence to prescribed treatments. In contrast, pyelonephritis prevention centers on avoiding urinary tract infections by practicing good hygiene, staying hydrated, and promptly addressing lower urinary tract symptoms. Patient education should emphasize recognizing early signs of infection, the importance of completing prescribed antibiotic courses, and adopting lifestyle modifications to reduce risk factors specific to each condition.
Glomerulonephritis Infographic
 libterm.com
libterm.com