Psoriasis is a chronic autoimmune condition characterized by rapid skin cell buildup, resulting in scaly, inflamed patches that often cause itching and discomfort. Effective management typically involves topical treatments, phototherapy, and systemic medications tailored to reduce flare-ups and improve your skin's health. Discover comprehensive strategies to control psoriasis symptoms and enhance your quality of life in the rest of this article.
Table of Comparison
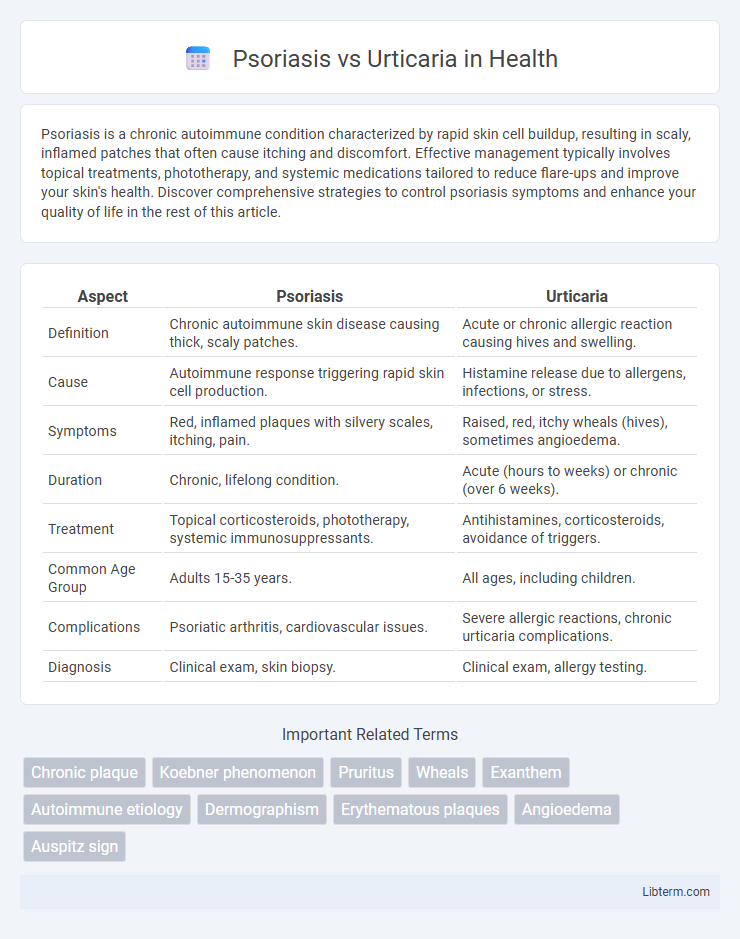
| Aspect | Psoriasis | Urticaria |
|---|---|---|
| Definition | Chronic autoimmune skin disease causing thick, scaly patches. | Acute or chronic allergic reaction causing hives and swelling. |
| Cause | Autoimmune response triggering rapid skin cell production. | Histamine release due to allergens, infections, or stress. |
| Symptoms | Red, inflamed plaques with silvery scales, itching, pain. | Raised, red, itchy wheals (hives), sometimes angioedema. |
| Duration | Chronic, lifelong condition. | Acute (hours to weeks) or chronic (over 6 weeks). |
| Treatment | Topical corticosteroids, phototherapy, systemic immunosuppressants. | Antihistamines, corticosteroids, avoidance of triggers. |
| Common Age Group | Adults 15-35 years. | All ages, including children. |
| Complications | Psoriatic arthritis, cardiovascular issues. | Severe allergic reactions, chronic urticaria complications. |
| Diagnosis | Clinical exam, skin biopsy. | Clinical exam, allergy testing. |
Introduction to Psoriasis and Urticaria
Psoriasis is a chronic autoimmune skin disorder characterized by rapid skin cell proliferation, resulting in thick, red, scaly patches commonly found on the elbows, knees, and scalp. Urticaria, also known as hives, is an acute or chronic condition marked by itchy, raised welts caused by histamine release in response to allergens or other triggers. Both conditions involve immune system dysfunction but differ significantly in pathophysiology, clinical presentation, and treatment approaches.
Understanding Psoriasis: Causes and Risk Factors
Psoriasis is a chronic autoimmune skin condition characterized by rapid skin cell turnover, leading to thick, scaly plaques, often caused by genetic predisposition, immune system dysfunction, and environmental triggers like stress or infections. Unlike urticaria, which results from histamine release causing transient hives, psoriasis involves persistent inflammation and overactive T-cells targeting the skin. Key risk factors for psoriasis include family history, smoking, obesity, and certain medications, differentiating its underlying autoimmune nature from the allergic reactions seen in urticaria.
Understanding Urticaria: Causes and Triggers
Urticaria, also known as hives, is characterized by sudden, itchy, red or skin-colored welts often caused by allergic reactions to foods, medications, insect stings, or infections. Unlike psoriasis, which is a chronic autoimmune disease leading to thick, scaly skin patches, urticaria results from histamine release triggered by immune responses or physical stimuli such as heat, pressure, or cold. Identifying specific allergens and environmental factors is crucial for effective management and prevention of urticaria flare-ups.
Key Differences Between Psoriasis and Urticaria
Psoriasis is a chronic autoimmune skin disease characterized by thick, red, scaly plaques primarily caused by rapid skin cell proliferation, whereas urticaria, or hives, presents as transient, itchy wheals resulting from allergic reactions or histamine release. Unlike psoriasis, which involves long-lasting lesions often on the scalp, elbows, and knees, urticaria lesions typically resolve within 24 hours and can appear anywhere on the body. Treatment for psoriasis often includes immunosuppressants and biologics targeting immune pathways, while urticaria management focuses on antihistamines and avoiding allergens.
Symptoms Comparison: Psoriasis vs Urticaria
Psoriasis presents with thick, red patches covered in silvery-white scales, often accompanied by itching and sometimes joint pain, predominantly appearing on the scalp, elbows, and knees. Urticaria, or hives, manifests as raised, itchy welts with varying sizes and shapes that rapidly appear and fade, frequently triggered by allergic reactions or stress. Unlike the chronic scaling of psoriasis, urticaria's symptoms are transient and usually resolve within hours to days without scaling or persistent skin changes.
Diagnostic Approaches for Psoriasis and Urticaria
Diagnostic approaches for psoriasis primarily involve clinical examination of characteristic erythematous plaques with silvery scales, supported by histopathological analysis from skin biopsies revealing epidermal hyperplasia and parakeratosis. In contrast, urticaria diagnosis is mainly clinical, emphasizing the identification of transient wheals and angioedema, with laboratory tests and allergen challenge used to exclude underlying triggers or autoimmune components. Dermoscopy and serological markers such as elevated IgE levels may aid in differentiating chronic urticaria from other dermatological conditions.
Treatment Options for Psoriasis
Treatment options for psoriasis include topical corticosteroids, vitamin D analogs, and phototherapy, which help reduce inflammation and slow skin cell growth. Systemic treatments such as methotrexate, cyclosporine, and biologics like adalimumab target the immune system to control severe or widespread psoriasis. Unlike urticaria, which primarily relies on antihistamines and identifying triggers, psoriasis treatment focuses on long-term management of chronic inflammation and skin cell proliferation.
Treatment Strategies for Urticaria
Treatment strategies for urticaria primarily involve antihistamines, which effectively reduce itching and wheals by blocking histamine receptors. In chronic cases, immunomodulatory agents such as omalizumab or corticosteroids may be prescribed to control persistent symptoms. Avoidance of known triggers combined with patient education enhances treatment efficacy and minimizes flare-ups.
Long-Term Management and Prognosis
Psoriasis requires long-term management with topical treatments, phototherapy, and systemic medications to control chronic inflammation and prevent flare-ups, with prognosis varying based on severity and response to therapy. Urticaria, often acute but sometimes chronic, typically involves antihistamines and avoidance of triggers, and its prognosis is generally favorable, though chronic cases may persist for months or years. Both conditions benefit from ongoing dermatologic evaluation to adjust treatments and monitor disease progression.
When to Seek Medical Advice
Seek medical advice for psoriasis when persistent red, scaly patches cause severe itching, pain, or joint stiffness, indicating potential psoriatic arthritis. Consult a healthcare provider for urticaria if hives are widespread, accompanied by difficulty breathing, swelling of the face or throat, or if they persist beyond six weeks, suggesting chronic urticaria. Immediate emergency care is necessary if urticaria triggers anaphylaxis or if psoriasis lesions become infected or significantly impair quality of life.
Psoriasis Infographic
 libterm.com
libterm.com