Epidural anesthesia provides targeted pain relief by injecting medication near the spinal cord, commonly used during labor and certain surgeries. This technique helps reduce discomfort while allowing you to remain awake and alert throughout the procedure. Discover how an epidural can impact your experience and what to expect in the full article.
Table of Comparison
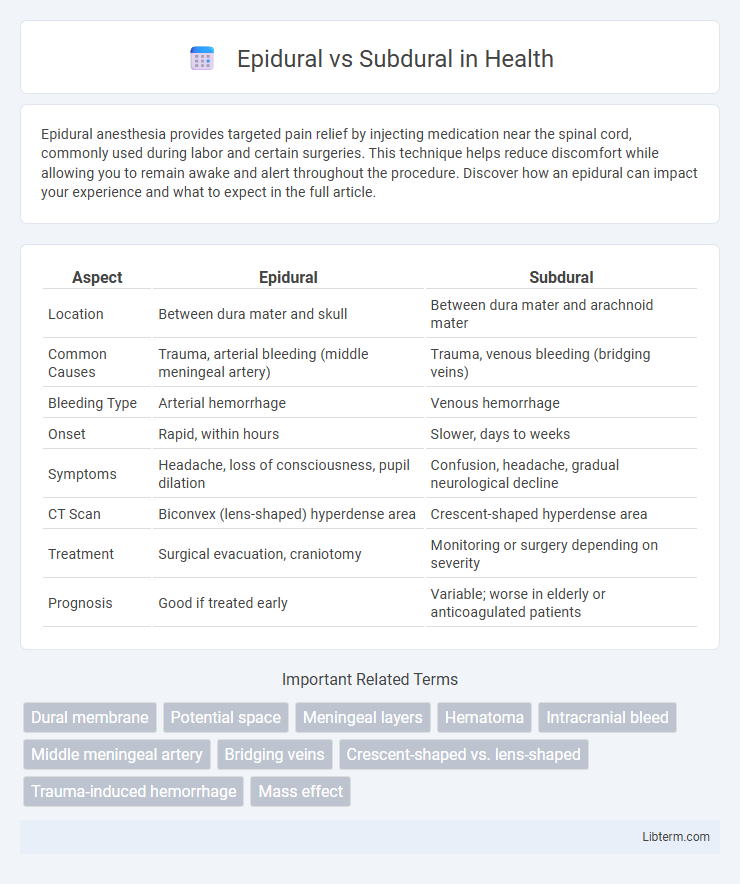
| Aspect | Epidural | Subdural |
|---|---|---|
| Location | Between dura mater and skull | Between dura mater and arachnoid mater |
| Common Causes | Trauma, arterial bleeding (middle meningeal artery) | Trauma, venous bleeding (bridging veins) |
| Bleeding Type | Arterial hemorrhage | Venous hemorrhage |
| Onset | Rapid, within hours | Slower, days to weeks |
| Symptoms | Headache, loss of consciousness, pupil dilation | Confusion, headache, gradual neurological decline |
| CT Scan | Biconvex (lens-shaped) hyperdense area | Crescent-shaped hyperdense area |
| Treatment | Surgical evacuation, craniotomy | Monitoring or surgery depending on severity |
| Prognosis | Good if treated early | Variable; worse in elderly or anticoagulated patients |
Introduction to Epidural and Subdural Spaces
The epidural space is the potential space between the dura mater and the vertebral wall, containing fat and blood vessels that cushion the spinal cord. In contrast, the subdural space lies between the dura mater and the arachnoid mater, typically a narrow, fluid-filled gap that becomes apparent mainly during pathological conditions. Understanding these anatomical differences is essential for procedures like epidural anesthesia and the diagnosis of subdural hematomas.
Anatomy: Epidural vs Subdural Regions
The epidural space is located between the outer dura mater and the inner surface of the skull or vertebral canal, containing fat, blood vessels, and connective tissue, which cushions the central nervous system. In contrast, the subdural space lies between the dura mater and the arachnoid mater, typically a potential rather than actual space, where subdural hematomas can accumulate following trauma. Understanding the distinct anatomical boundaries of the epidural and subdural regions is critical for diagnosing and managing cranial and spinal injuries effectively.
Causes of Epidural and Subdural Hematomas
Epidural hematomas typically result from traumatic injury causing arterial bleeding, often from the middle meningeal artery due to skull fractures. Subdural hematomas arise primarily from head trauma causing venous bleeding, specifically the tearing of bridging veins between the brain surface and dura mater. Both conditions involve intracranial bleeding but differ in source vessels and injury mechanisms, impacting diagnosis and treatment strategies.
Clinical Symptoms: Differentiating Features
Epidural hematomas typically present with a brief loss of consciousness followed by a lucid interval before neurological deterioration, characterized by ipsilateral pupil dilation and contralateral hemiparesis due to arterial bleeding between the dura mater and skull. Subdural hematomas often manifest with a more gradual onset of symptoms such as headache, confusion, decreased level of consciousness, and focal neurological deficits caused by venous bleeding between the dura and arachnoid mater. Distinguishing features include rapid symptom progression and pupil asymmetry in epidural hematomas versus slower progression and fluctuating consciousness in subdural hematomas, influencing emergent diagnosis and management.
Diagnostic Imaging Techniques
Diagnostic imaging techniques for differentiating epidural and subdural hematomas primarily include computed tomography (CT) and magnetic resonance imaging (MRI). Epidural hematomas typically appear as biconvex (lentiform) hyperdense collections on CT scans, confined by suture lines, whereas subdural hematomas present as crescent-shaped, crescentic hyperdense or hypodense collections that can cross sutures but are limited by dural reflections. MRI, especially using T1 and T2-weighted sequences, offers enhanced sensitivity in detecting subacute or chronic hematomas, providing superior contrast resolution to distinguish blood products and identify associated brain injuries.
Risk Factors and Patient Demographics
Epidural hematomas primarily affect younger adults and are commonly linked to traumatic injury involving arterial bleeding, especially from the middle meningeal artery, with risk factors including skull fractures and rapid head trauma. Subdural hematomas are more prevalent in older adults and individuals with brain atrophy, frequently resulting from venous bleeding due to tearing of bridging veins, with risk factors such as anticoagulant use, alcohol abuse, and falls. Both conditions require prompt diagnosis, but subdural hematomas tend to develop more slowly and are often associated with chronic conditions affecting vulnerable populations.
Treatment and Management Options
Epidural hematomas typically require urgent surgical intervention such as burr hole drainage or craniotomy to remove the accumulated blood and relieve pressure on the brain. Subdural hematomas may be managed conservatively with close neurological monitoring if small and asymptomatic, but larger or symptomatic subdural hematomas often necessitate surgical evacuation through craniotomy or twist-drill craniostomy. Medical management for both includes controlling intracranial pressure using mannitol or hypertonic saline and addressing underlying causes to optimize patient outcomes.
Prognosis and Potential Complications
Epidural hematomas typically present a better prognosis with prompt surgical intervention, as they involve arterial bleeding between the dura mater and the skull, which can rapidly expand but is often localized. Subdural hematomas, characterized by venous bleeding beneath the dura mater, carry a higher risk of complications such as increased intracranial pressure, brain herniation, and chronic neurological deficits due to their tendency to develop more insidiously and affect the brain tissue directly. Both conditions require urgent medical evaluation, but subdural hematomas often result in more severe long-term cognitive and motor impairment compared to epidural hematomas.
Prevention Strategies and Best Practices
Effective prevention strategies for epidural and subdural hematomas primarily include the use of protective headgear in high-risk activities like contact sports and construction work. Best practices involve early detection through regular neurological assessments and prompt imaging techniques such as CT scans following head trauma to mitigate complications. Ensuring patient education on avoiding falls and alcohol moderation also plays a critical role in reducing incidence rates.
Conclusion: Key Differences Between Epidural and Subdural Conditions
Epidural hematomas occur between the dura mater and the skull, often caused by arterial bleeding, while subdural hematomas form between the dura mater and the arachnoid layer, typically resulting from venous bleeding. Epidural conditions usually present rapidly with a lucid interval followed by severe symptoms, whereas subdural hematomas develop more gradually with fluctuating consciousness levels. Accurate diagnosis through imaging and understanding these distinct anatomical and clinical characteristics are crucial for effective treatment and prognosis.
Epidural Infographic
 libterm.com
libterm.com